Overview
Navigating weight management can be challenging, and understanding your insurance coverage is a crucial step. This article explores whether United Healthcare covers Wegovy, a medication designed to assist in weight management. It’s important to note that coverage can vary significantly based on specific insurance plans and medical criteria, which may leave you feeling uncertain.
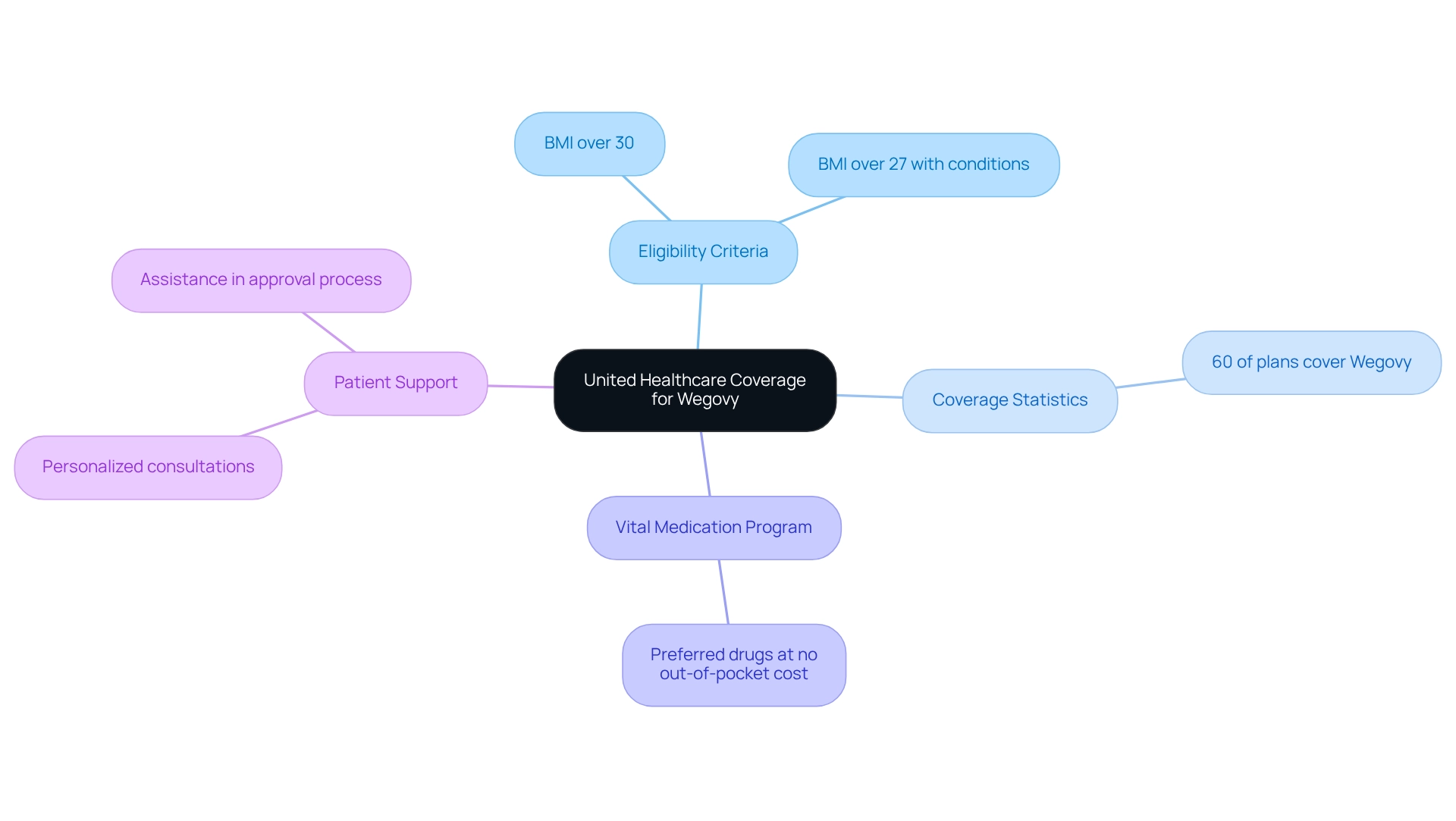
Approximately 60% of United Healthcare plans do offer benefits for Wegovy, but this is contingent upon meeting certain eligibility criteria, such as BMI thresholds. This means that taking the time to understand the details of your individual plan is essential. By doing so, you can better navigate potential out-of-pocket costs and the approval processes that may arise.
We’re here for you as you embark on this journey. Remember, understanding your options is a powerful step toward achieving your weight management goals. Together, we can explore the possibilities that lie ahead.
Introduction
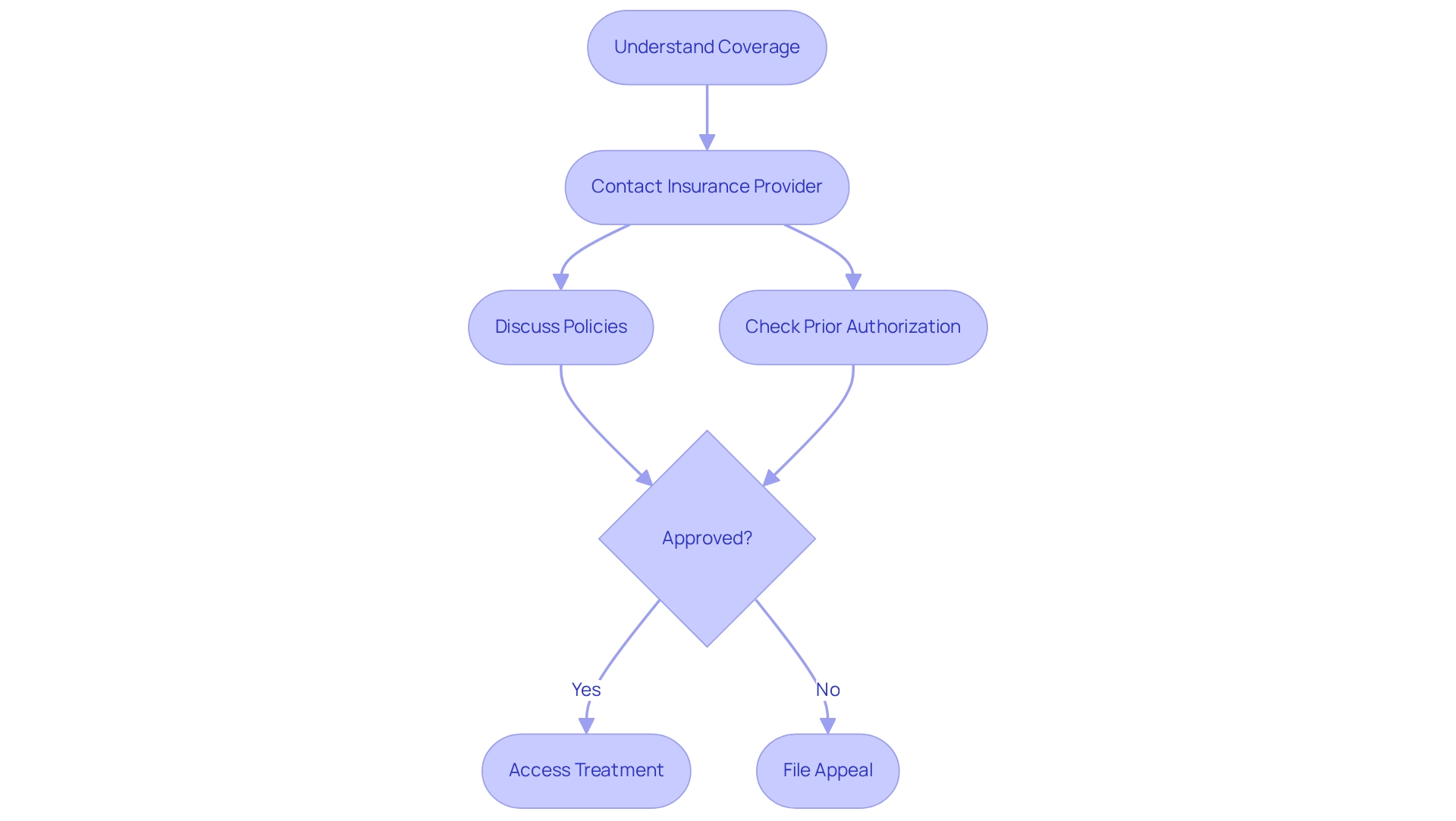
In the realm of weight management, we understand that the journey can feel overwhelming. The landscape is rapidly evolving, especially with the emergence of medications like Wegovy, which offer hope to many. As individuals seek effective solutions to combat obesity and its related health issues, navigating the intricacies of insurance coverage becomes crucial. Have you ever felt lost in a maze of policies? From prior authorization requirements to formulary lists, patients face a complex web that can significantly impact their access to this groundbreaking treatment.
This article aims to illuminate the various facets of Wegovy coverage. We will explore the criteria needed for approval, discuss the appeal process for denied claims, and highlight the role of personalized support in enhancing your weight loss journey. By equipping you with essential knowledge, we empower you to advocate for your health and make informed decisions in your pursuit of wellness. Together, we can achieve your goals and navigate this path with confidence.
Minimal: Personalized Weight Loss Solutions Including Wegovy Coverage
At Minimal, we understand that embarking on a weight loss journey can feel overwhelming. That’s why we are committed to offering transformative solutions for loss, incorporating medications like semaglutide into a comprehensive health strategy tailored just for you, and we can help you find out if united healthcare does cover wegovy. Our expert team is here to provide personalized coaching and comprehensive support, ensuring that you receive care that aligns with your individual health goals while we explore if united healthcare does cover wegovy, which is essential for successful weight management. We believe that every step you take towards your health is significant, and we’re here to support you on this path. With options starting at just $99.99/month, Minimal empowers you to begin your health journey without the limitations often imposed by insurance.
Together, we can achieve your goals. Let us help you transform your health with compassion and understanding.
United Healthcare: Coverage Policies for Wegovy Explained
The question of whether United Healthcare covers Wegovy can vary significantly based on specific insurance plans. Typically, individuals who meet certain medical criteria, such as a body mass index (BMI) over 30 or a BMI over 27 with related health conditions, may wonder, does United Healthcare cover Wegovy? As of 2025, approximately 60% of United Healthcare plans offer benefits for this medication, prompting inquiries about whether does United Healthcare cover Wegovy, which reflects a growing acceptance of weight loss treatments within insurance systems. Notably, the Vital Medication Program provides specific categories of preferred drugs at no out-of-pocket expense, which may include options for individuals seeking Wegovy.
We encourage patients to carefully examine their specific plan details to understand the scope of benefits and any potential out-of-pocket expenses related to the medication, specifically to find out if does United Healthcare cover Wegovy, which is priced at around $1,350 monthly. Many individuals have successfully navigated the complexities of insurance, often with the assistance of healthcare professionals who help in the approval process. At Minimal, we’re here for you, offering personalized consultations to help you understand your options and navigate these challenges effectively.
Expert opinions emphasize that meeting medical criteria is vital for obtaining coverage. Insurance specialists suggest that if more insurers and pharmacy benefits managers adopt similar strategies, it could lead to greater acceptance of weight loss medications, ultimately supporting patients in their search for effective treatment options. This evolving landscape highlights the importance of personalized care, as demonstrated by case studies from Minimal, where dedicated care teams, including physicians like Dr. Chance Miller, enhance client satisfaction and contribute to successful health transformations. Positive feedback from customers, such as Deborah N., a verified buyer who praised her experience with Minimal, reinforces the effectiveness of our personalized health solutions. As Julie Stich, vice president of content at IFEBP, wisely notes, “If more insurers and pharmacy benefits managers pursue similar efforts, their affiliated health plans could become more open to covering weight loss drugs, knowing that their risk will be limited in that way.
Insurance Landscape: How Different Plans Cover Wegovy
Navigating the insurance landscape for weight loss medications can feel overwhelming, particularly when trying to find out does United Healthcare cover Wegovy. It’s important to recognize that benefits can vary significantly among health insurance companies. Some plans may offer complete coverage for the medication, while others might require prior approval or impose limitations like step therapy. This means that individuals may need to try alternative treatments before gaining access to the drug.
We encourage patients to carefully review their insurance provider’s formulary to determine if the medication is included and to understand any specific conditions for coverage, especially to find out does United Healthcare cover Wegovy. Recent statistics show a positive trend: beneficiaries diagnosed with obesity or overweight, especially those with a history of heart attacks or strokes, are increasingly being recognized as eligible for this treatment. This change reflects a growing acknowledgment of the medication’s role in managing weight-related health issues, as it mimics the GLP-1 hormone to help regulate appetite and promote feelings of fullness.
However, the variability in coverage remains a significant concern, particularly regarding whether United Healthcare covers Wegovy, with some plans imposing higher out-of-pocket costs or limiting access based on medical necessity criteria. As the insurance landscape for weight loss medications evolves, healthcare analysts point out that coverage can differ dramatically even among major providers. For instance, while some insurance firms may cover the medication under specific conditions, it’s important to ask does United Healthcare cover Wegovy, as others might not include it at all.
This inconsistency can lead to disparities in access for individuals seeking support on their weight loss journey, especially when considering whether United Healthcare does cover Wegovy, as one person may find that their plan fully covers the medication, while another could face challenges like high copays or the need for extensive documentation to justify its use.
It’s also crucial to remember that this medication requires monitoring and guidance from healthcare professionals, highlighting the importance of professional oversight. Starting in 2025, understanding these distinctions will be vital for those pursuing effective management solutions through the medication, which has shown significant weight loss when combined with a lower-calorie diet and increased physical activity.
Proactive communication with insurance representatives can help manage the complexities of coverage, particularly regarding whether does United Healthcare cover Wegovy. Additionally, typical side effects of this medication may include nausea, diarrhea, vomiting, constipation, abdominal pain, headache, fatigue, dizziness, and low blood sugar in individuals with type 2 diabetes. It’s essential for patients to be aware of potential gallbladder issues, such as gallstones, which may require surgical intervention. Symptoms to watch for include upper abdominal pain and jaundice.
A thorough understanding of both insurance coverage and possible health effects is crucial for individuals considering this medication as part of their management approach. Remember, we’re here for you, and together, we can navigate these challenges to find the best solutions for your health.
Coverage Criteria: What You Need to Qualify for Wegovy
If you’re seeking assistance with medication, it’s important to know that demonstrating medical necessity is often a key step. This usually involves having a BMI of 30 or above, or a BMI of 27 or above if you have related health issues like diabetes or hypertension.
The FDA-approved GLP-1 injection containing semaglutide is a promising option for weight management, helping to improve health markers associated with obesity, and it is important to know if United Healthcare covers Wegovy, as you may need documentation from your healthcare provider to support your claim for benefits. This ensures that you meet the necessary criteria set by your insurance plan.
Remember, by following these guidelines, you can access this valuable treatment as part of a holistic approach to wellness.
We’re here for you, and this journey can be complemented by services offered by Minimal, such as personalized fitness training and nutrition consultations. Together, we can achieve your goals and support you in your path to better health.
Appeal Process: Steps to Challenge Wegovy Coverage Denials
Appeal Process: Steps to Challenge Coverage Denials for the Medication
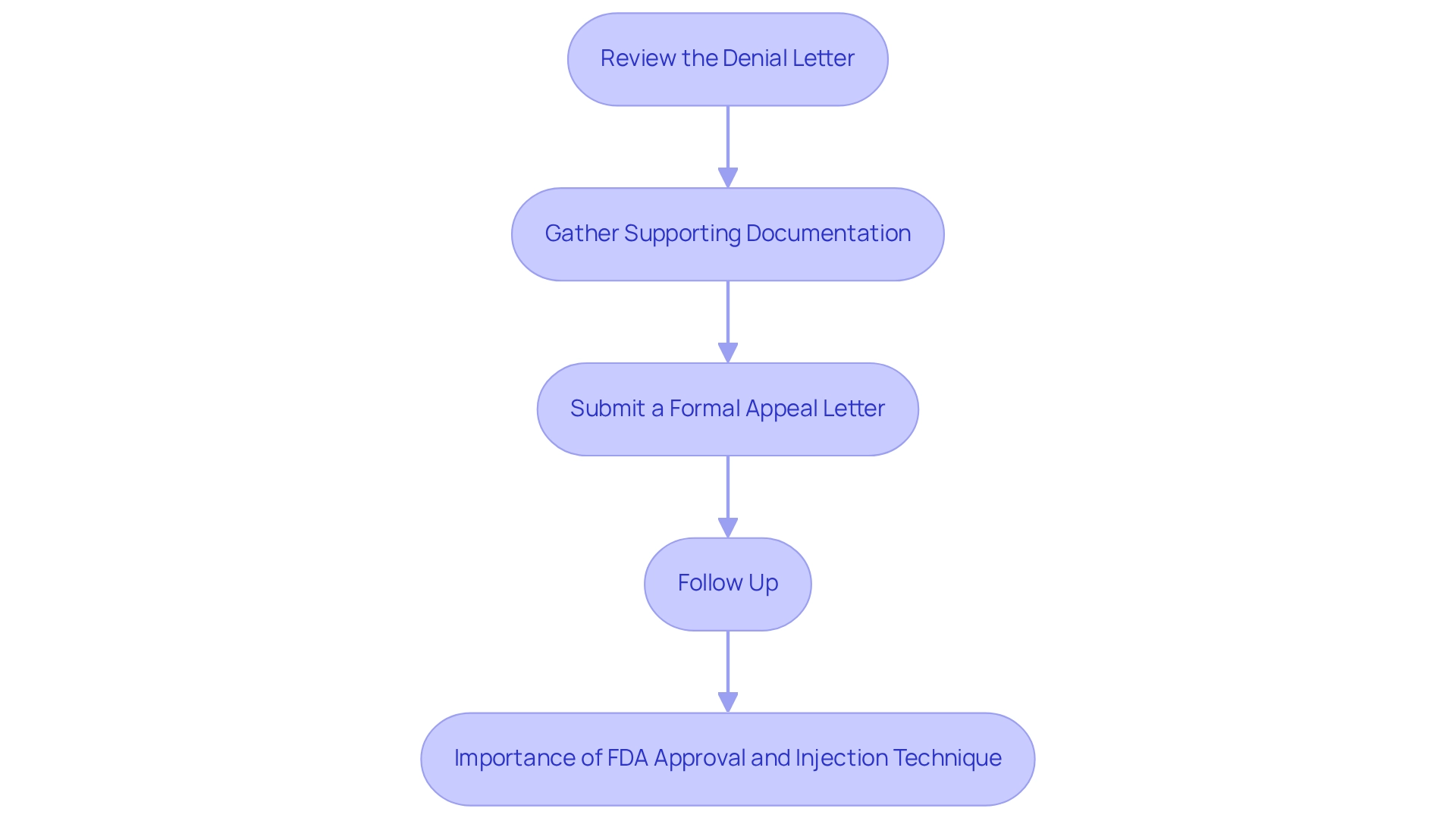
If you’ve faced a denial for your medication coverage, know that you have the right to appeal this decision. It’s understandable to feel overwhelmed, but we’re here to guide you through the process. Here’s how you can take action:
- Review the Denial Letter: Take a moment to check for the specific reasons behind the denial. Understanding these details is crucial.
- Gather Supporting Documentation: Collect your medical records and letters from healthcare providers. This documentation will strengthen your case and provide clarity.
- It’s essential to highlight that this FDA-approved medication containing semaglutide, specifically Wegovy, raises the question of whether United Healthcare covers Wegovy, as it not only aids in weight management but also enhances health markers associated with obesity.
- Submit a Formal Appeal Letter: Craft a detailed appeal letter to your insurance company, ensuring you include all necessary documentation.
- Follow Up: Don’t hesitate to contact your insurance provider to expedite the review process. Your persistence can make a difference, particularly in determining whether United Healthcare covers Wegovy, which is administered once a week via an injection pen that can be used on the abdomen, thigh, or upper arm. Remember, it’s crucial to follow your doctor’s guidance on proper dosage and injection techniques, including rotating injection sites to avoid irritation. Together, we can navigate this journey and achieve your health goals.
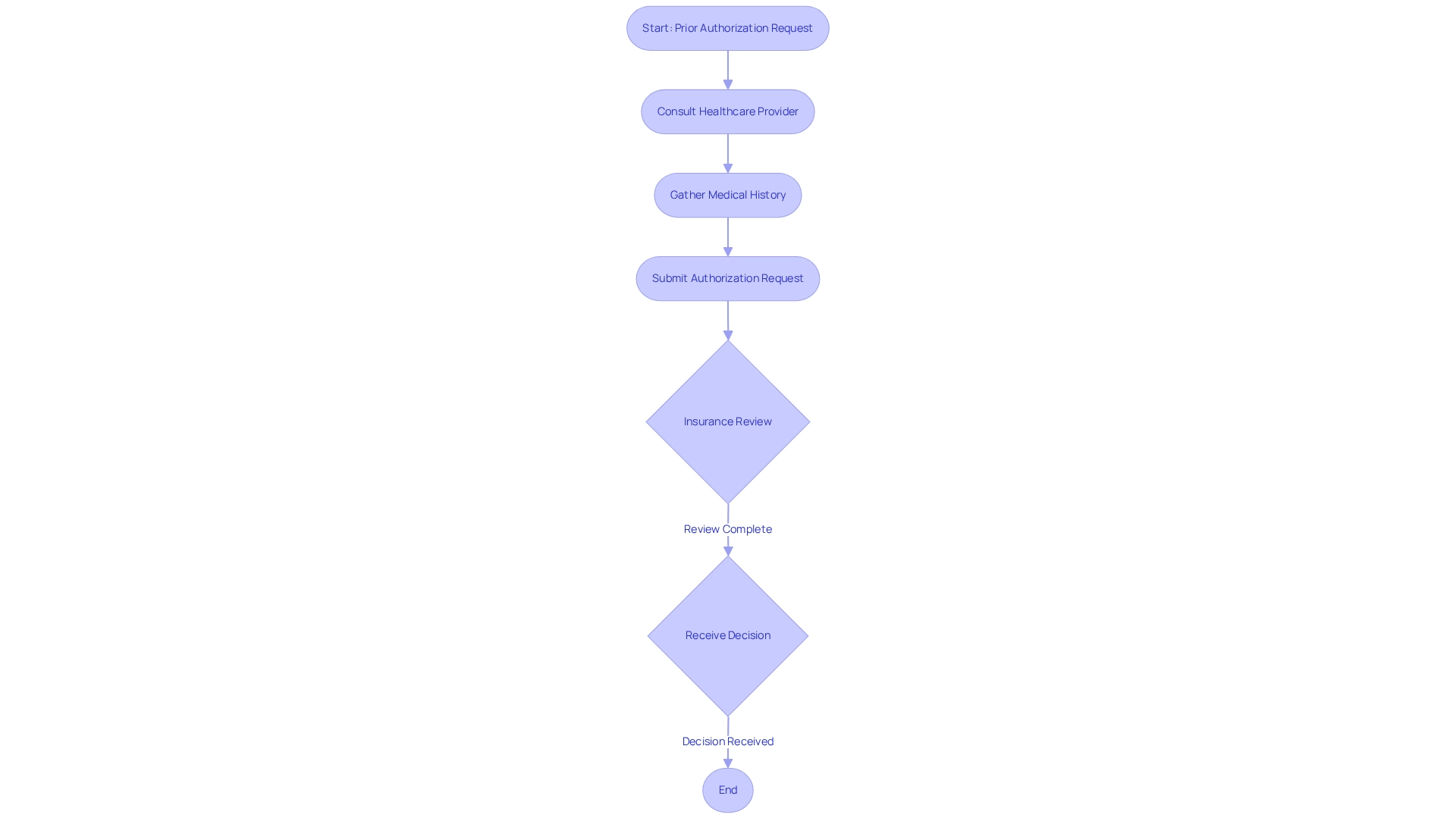
Prior Authorization: Navigating Wegovy Coverage Requirements
Navigating insurance plans can be challenging, especially when it comes to prior authorization for medications. This means that healthcare providers must submit a request to the insurance company before coverage can begin. It’s important to illustrate the medical necessity of the drug based on your unique health status and treatment history. This is particularly crucial for those who are overweight or obese, as they may face associated medical conditions like high blood pressure or type 2 diabetes.
Working closely with your healthcare provider is essential. Together, you can ensure that all necessary information is included in the prior authorization request, helping to avoid any delays in your treatment. One FDA-approved medication that may be beneficial is semaglutide, a GLP-1 receptor agonist. This medication is designed to help regulate appetite and food intake, making it a vital option for effective weight management.
Semaglutide is administered once a week using an injection pen on the abdomen, thigh, or upper arm. It’s crucial to rotate your injection sites to prevent irritation. Following your doctor’s guidance on dosage and administration can significantly enhance your results. Many clients begin to notice improvements within just a few weeks, but remember, it may take a few months to experience the full benefits. Together, we can achieve your goals and support you on this journey.
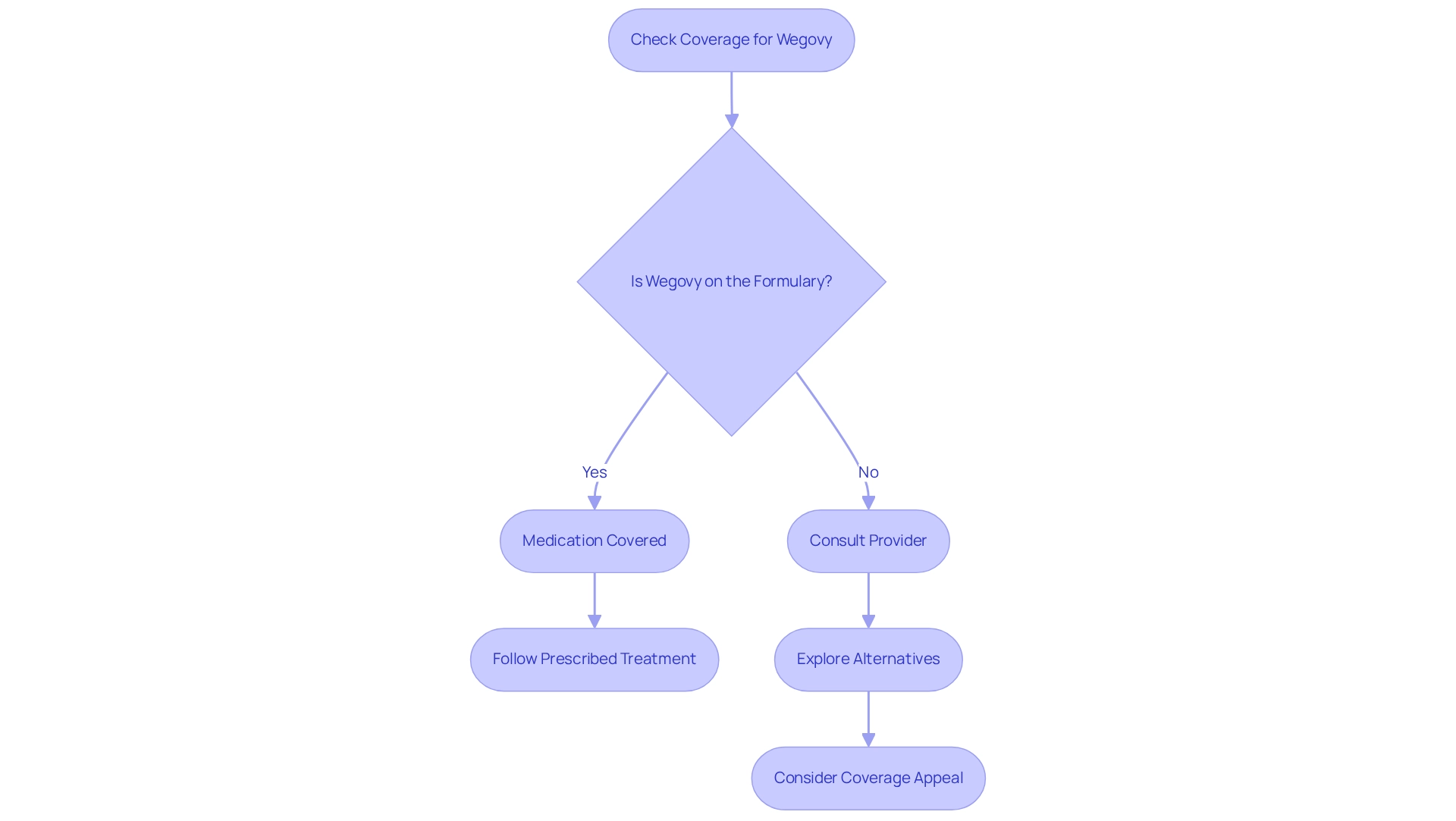
Formulary Lists: Checking Wegovy’s Status with Your Insurance
Navigating the complexities of medication coverage can feel overwhelming, but understanding whether United Healthcare covers Wegovy is a crucial step in your weight management journey. To find out if your medication is covered, specifically if does United Healthcare cover Wegovy, we encourage you to consult your provider’s formulary list. This list not only shows which medications are available but also categorizes them into tiers, which can significantly impact your out-of-pocket expenses.
For those considering a prescription drug containing semaglutide, it’s important to know that it’s designed to assist adults who are overweight or obese, particularly those facing related medical challenges. If you find that your medication isn’t listed, don’t hesitate to explore alternative options with your healthcare provider or think about appealing the coverage decision. Remember, you are not alone in this process.
Recent insights reveal that a common question is, does United Healthcare cover Wegovy, as more insurance plans are beginning to include this medication in their formularies, reflecting a positive shift in response to the increasing demand for effective weight management solutions. In fact, research indicates that as many as 70% of major health plans now offer coverage for this medication, leading to the question of does United Healthcare cover Wegovy?. This growing acceptance is a hopeful sign for those seeking support.
Moreover, Bernie Sanders, chair of the Senate health committee, recently stated, “I am pleased to share today that I have obtained written commitments from all the major PBMs that if Novo Nordisk were to significantly lower the list price for Ozempic and Wegovy, they would not restrict access.” This highlights the potential for changes in coverage based on pricing adjustments, which could benefit many individuals.
As you navigate this journey, be aware that initial prior authorization requests for Zepbound, especially for conditions like obstructive sleep apnea, may require supporting medical records. This step is vital for ensuring you receive the necessary support from your insurance provider.
We encourage you to frequently review your formulary status. By doing so, you can make informed decisions about your treatment options and ensure you receive the essential support for your health journey. Remember, together, we can achieve your goals, and we’re here for you every step of the way.
Out-of-Pocket Costs: What to Expect with Wegovy Coverage
We understand that out-of-pocket expenses for medication can be a source of concern, especially as you navigate your weight loss journey. The costs can vary significantly based on your insurance plan, including factors like deductibles, copayments, and whether United Healthcare covers Wegovy, as well as if the medication is on the formulary. It’s important to consult your insurance provider to get an estimate of your potential out-of-pocket expenses. Have you explored any available savings programs or discounts that might help reduce these costs?
At Minimal, while we do not accept insurance, we do offer HSA/FSA payment options for our services. This provides a flexible payment solution for our clients, helping to ease some of the financial burden. We want you to feel supported every step of the way.
Additionally, rest assured that we are completely HIPAA compliant, meaning your personal health information is securely managed and safeguarded as you progress through your journey. Remember, we’re here for you, and together, we can achieve your goals.
Employer-Sponsored Plans: How They Affect Wegovy Coverage
Your access to Wegovy can be significantly affected by whether United Healthcare covers Wegovy in employer-sponsored health plans. While some employers may provide extensive support for weight loss medications, others might impose limitations or exclude them altogether, which leads to the question: does United Healthcare cover Wegovy? Have you taken a moment to review your benefits package? Consulting with your HR department can help you understand the specifics of your plan, including any options for appealing if coverage is denied.
At Minimal, we understand that navigating weight loss can be overwhelming, and we’re here for you. We offer holistic solutions for weight management, including compounded Tirzepatide, designed to empower your health journey through personalized care and comprehensive support. Our dedicated team is ready to guide you every step of the way, providing tailored fitness and nutrition plans, along with regular check-ins to track your progress. Together, we can ensure you have the resources you need for effective weight loss.
Key Takeaways: Essential Facts About Wegovy Coverage
Navigating the benefits of Wegovy can feel overwhelming, but understanding whether United Healthcare does cover Wegovy, along with your insurance provider’s specific policies, qualification criteria, and potential out-of-pocket expenses, is key. We encourage you to actively communicate with your healthcare providers and insurance representatives to tackle the complexities of benefits, such as prior authorization and formulary checks. Knowing the appeal process is essential; it empowers you to advocate effectively for your treatment choices.
Many individuals have successfully managed these challenges, with numerous patients sharing positive experiences in accessing Wegovy. For instance, data from over 70,000 patients involved in management programs show a high success rate in achieving weight loss objectives, underscoring the importance of persistence in navigating insurance issues.
Healthcare specialists emphasize that understanding the intricacies of insurance, such as does United Healthcare cover Wegovy, can significantly impact your treatment accessibility. As Melisa Horton, a PharmD and Strategic Pharmacy Consultant, aptly states, “This largely depends on if this aligns with your company’s culture and what your people value.” This highlights the importance of aligning treatment options with employer policies to enhance your chances of success.
Looking ahead to 2025, statistics reveal that employers are increasingly exploring strategies like prior authorization and management programs to manage expenses related to GLP-1 medications such as Wegovy. This trend is crucial for you, as it may influence whether United Healthcare covers Wegovy and affect the overall affordability of treatment.
If you’re seeking personalized support, connecting with Minimal is both easy and beneficial. You can reach out via phone at (872) 228 – 2358 or email [email protected]. Our loss program starts with a consultation to assess your health and determine the best treatment strategy, including potential prescription options like Semaglutide. We combine medication with personalized fitness and nutrition plans, along with holistic health strategies, to support your long-term success.
Recent news suggests that state regulations limiting off-label drug use are unlikely to face significant obstacles, which may impact accessibility dynamics and individual access to treatment. Overall, staying informed about whether United Healthcare covers Wegovy and actively engaging in discussions with healthcare providers can lead to better outcomes for patients like you seeking effective weight loss solutions.
Conclusion
Understanding the intricacies of Wegovy coverage is essential for anyone navigating the challenges of weight management. Have you ever felt overwhelmed by the complexities of insurance? From eligibility criteria to the appeal process for denied claims, this article has illuminated the critical steps needed to secure access to this groundbreaking medication. With insurance coverage varying significantly across different providers, it is imperative for patients to familiarize themselves with their specific plans, including prior authorization requirements and formulary lists.
Moreover, the importance of personalized support cannot be overstated. Engaging with healthcare professionals and organizations like Minimal can provide tailored guidance and resources that enhance your weight loss journey. As you work to overcome barriers to coverage, proactive communication with insurance representatives and healthcare providers will be vital in advocating for your treatment options.
Ultimately, as the landscape of weight loss medications continues to evolve, staying informed and persistent will empower you to make educated decisions about your health. By understanding the nuances of Wegovy coverage and utilizing available support systems, you can confidently pursue your weight management goals and improve your overall well-being. Remember, we’re here for you, and together, we can achieve your goals.
Frequently Asked Questions
What is Minimal’s approach to weight loss?
Minimal offers transformative solutions for weight loss, incorporating medications like semaglutide into a comprehensive health strategy tailored to individual needs, along with personalized coaching and support.
Does United Healthcare cover Wegovy?
Coverage for Wegovy by United Healthcare varies based on specific insurance plans. As of 2025, approximately 60% of United Healthcare plans offer benefits for this medication, particularly for individuals with a BMI over 30 or over 27 with related health conditions.
What are the eligibility criteria for Wegovy coverage?
Individuals typically need to meet certain medical criteria, such as having a BMI over 30 or a BMI over 27 with related health issues, to be considered for coverage of Wegovy.
What should patients do to understand their coverage for Wegovy?
Patients are encouraged to carefully review their specific insurance plan details and formulary to determine if Wegovy is included and to understand any conditions for coverage.
What are the potential costs associated with Wegovy?
Wegovy is priced at around $1,350 monthly, and while some plans may cover it fully, others might impose higher out-of-pocket costs or require prior approval.
How can patients navigate the complexities of insurance coverage for Wegovy?
Proactive communication with insurance representatives and seeking assistance from healthcare professionals can help patients manage the complexities of coverage and understand their options.
What are common side effects of Wegovy?
Common side effects may include nausea, diarrhea, vomiting, constipation, abdominal pain, headache, fatigue, dizziness, and low blood sugar in individuals with type 2 diabetes. Patients should also be aware of potential gallbladder issues, such as gallstones.
Why is professional oversight important when using Wegovy?
Professional oversight is crucial as the medication requires monitoring and guidance from healthcare professionals to ensure safe and effective use, especially in conjunction with a lower-calorie diet and increased physical activity.