Overview
Navigating insurance coverage for GLP-1 medications can feel overwhelming, but you’re not alone in this journey. Start by reviewing your coverage policy to understand the specific requirements, such as prior authorization and medical necessity documentation. It’s essential to prepare thoroughly and communicate openly with both your insurance provider and healthcare professionals.
Have you considered exploring financial assistance programs? These can significantly alleviate the costs associated with your treatment, making it easier to focus on your health. Remember, taking these steps not only enhances your chances of obtaining coverage but also empowers you in your weight loss journey.
Together, we can achieve your goals. With the right support and resources, you can navigate this process with confidence. You’re taking an important step towards better health, and we’re here for you every step of the way.
Introduction
Navigating the complexities of insurance coverage for GLP-1 medications can feel overwhelming, especially for those seeking effective treatments for obesity and diabetes. It’s important to recognize the nuances of insurance policies, prior authorization requirements, and potential financial assistance, as these factors can significantly influence a patient’s access to these vital medications.
With many claims facing denial, how can you ensure that you secure the necessary coverage? This guide offers essential strategies and insights designed to empower you to overcome obstacles and successfully obtain GLP-1 medications through your insurance plans. Together, we can navigate this journey towards better health.
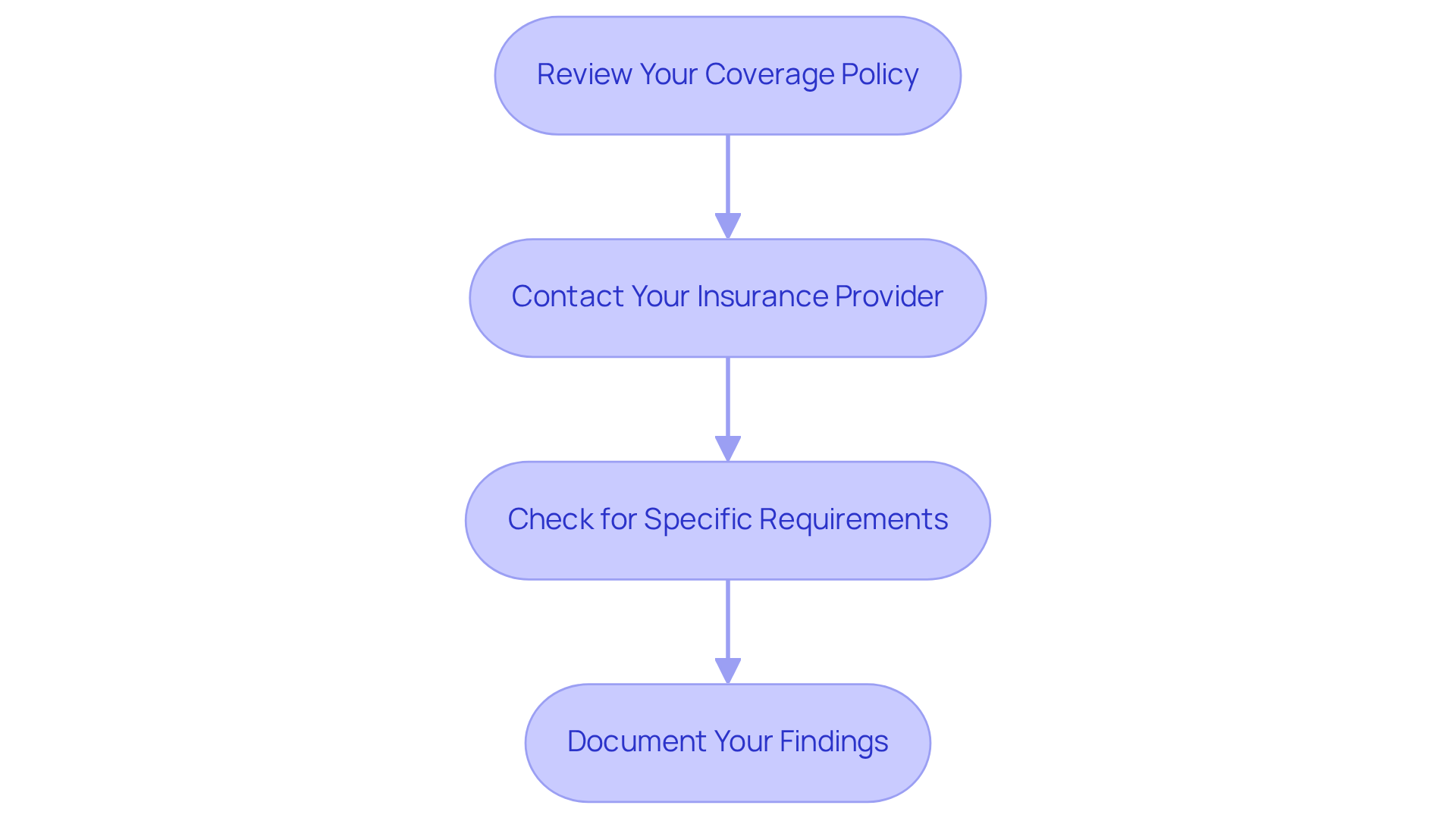
Assess Your Insurance Coverage for GLP-1 Medications
-
Review Your Coverage Policy: Start by locating your policy documents, and take a moment to identify the section that outlines your prescription drug coverage. This section usually includes a formulary list, detailing which drugs are covered. Understanding this can help you feel more secure in your choices.
-
Contact Your Insurance Provider: If anything remains unclear, don’t hesitate to reach out to the customer service number on your insurance card. When you call, specifically inquire how to get GLP-1 covered by insurance for treatments like Ozempic® and Wegovy®. It’s important to clarify whether these medications are covered for weight management or strictly for diabetes treatment, as this can significantly impact your options.
-
Check for Specific Requirements: Many insurance plans have specific criteria for benefits. This might include a documented history of obesity or related health conditions. During your call, make sure to inquire about these requirements. Understanding what paperwork you may need can empower you on your journey.
-
Document Your Findings: Keep a thorough record of your discussions and any written correspondence related to your insurance. This documentation will be invaluable if you need to appeal a denial or clarify policy details later on. Remember, you are not alone in this process.
Currently, around 50 million adult Americans have insurance for anti-obesity treatments, yet only a small portion of large firms provide support for GLP-1 drugs. It’s essential to comprehend your coverage plan, as 79% of firms that offer weight loss medications require insured members to fulfill specific conditions for approval. By following these steps, you can navigate the complexities of GLP-1 treatments with confidence and clarity. Together, we can achieve your goals.
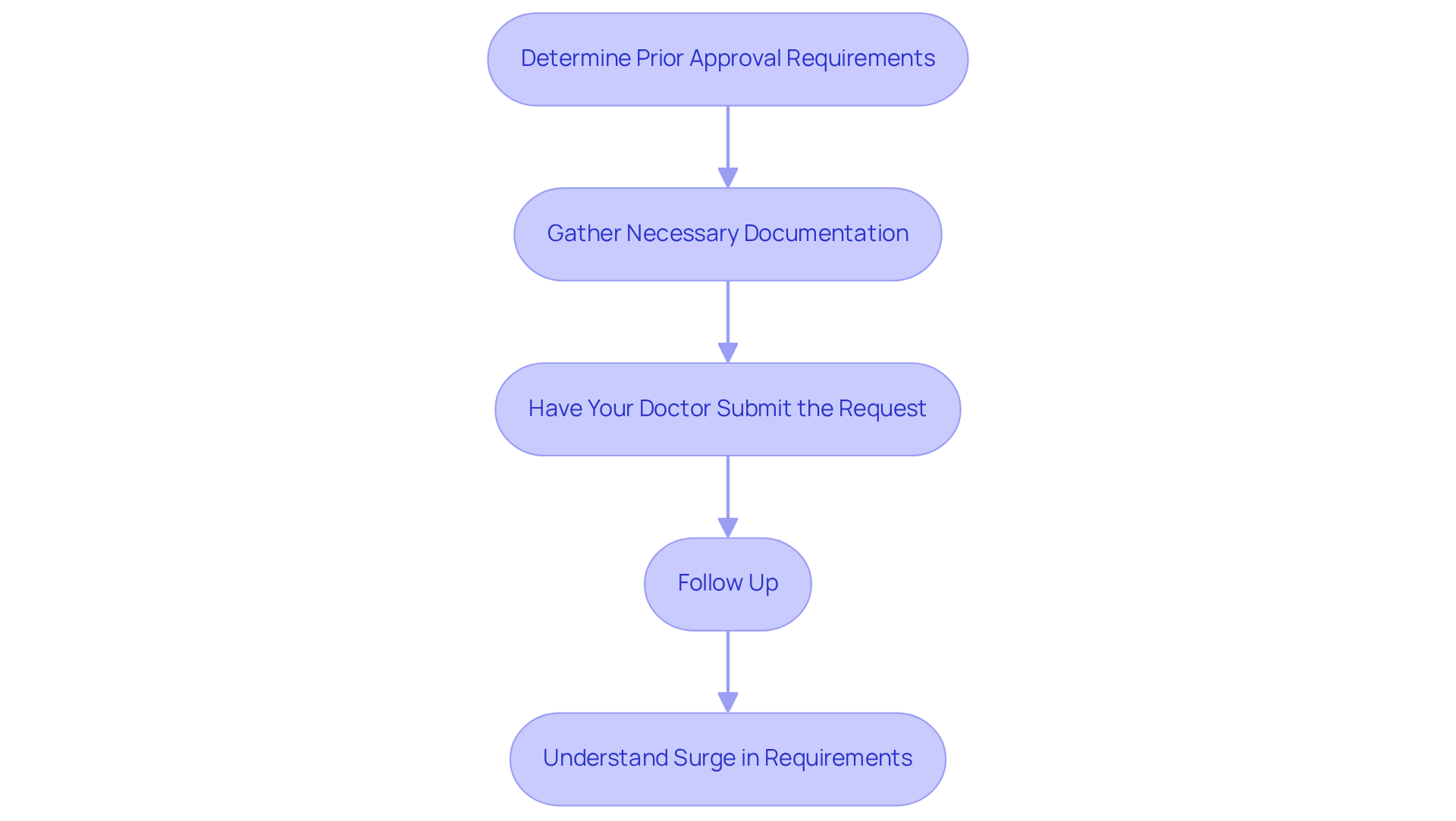
Understand Prior Authorization Requirements
Navigating the complexities of how to get GLP-1 covered by insurance for GLP-1 treatments can feel overwhelming, but understanding prior authorization requirements is essential to your journey. Here’s how you can effectively manage the process:
-
Determine Prior Approval Requirements: Start by checking with your coverage provider to see if prior authorization is necessary for GLP-1 treatments. You can usually find this information in your insurance policy or formulary.
-
Gather Necessary Documentation: Collect medical records that demonstrate the medical necessity of the medication. Important documents might include your Body Mass Index (BMI), weight history, and records of any previous weight management treatments you’ve tried. Remember, understanding how to get GLP-1 covered by insurance typically involves knowing that most insurers require a BMI of 30 or higher, or 27 with a qualifying comorbidity, to approve coverage.
-
Have Your Doctor Submit the Request: Your healthcare provider will typically need to submit the prior authorization request on your behalf. Make sure they include all required documentation, such as a detailed letter of medical necessity and recent health metrics, to bolster your case.
-
Follow Up: After submission, it’s important to follow up with your insurance company to check the status of your prior authorization request. Processing times usually range from 5 to 10 business days, so staying in contact is crucial.
It’s worth noting that prior authorization requirements for GLP-1 medications have surged, with over 80% of claims now requiring this step. Successful requests for how to get GLP-1 covered by insurance often hinge on thorough records and clear communication between patients and healthcare providers. For instance, many denials can be overturned on appeal when stronger documentation is provided, underscoring the importance of thorough preparation.
As healthcare professionals emphasize, prompt access to these treatments is vital for effective weight management. Remember, you are not alone in this process; together, we can achieve your goals, making the prior authorization process a crucial step in your health journey.
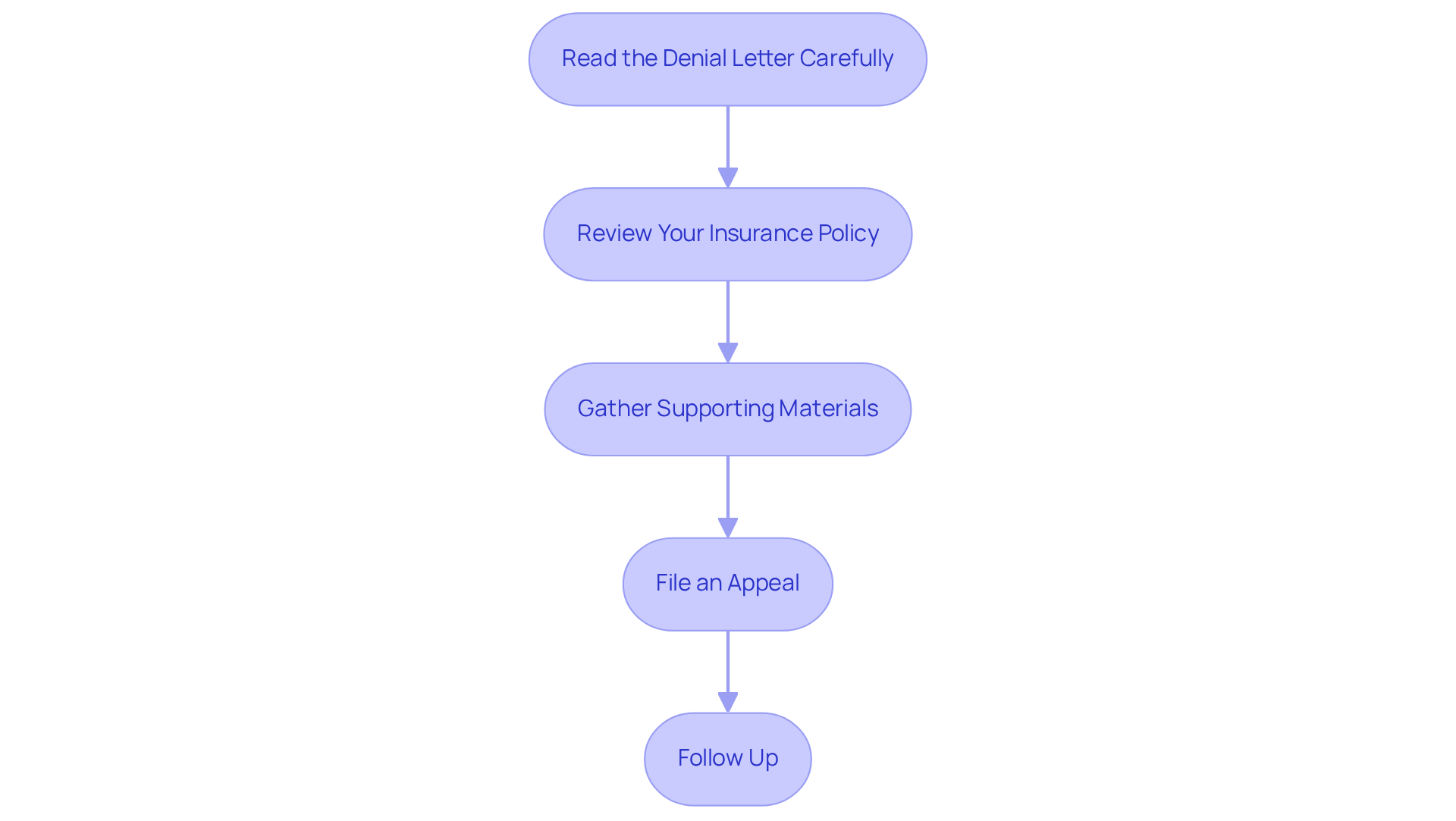
Manage Insurance Denials and Appeals
-
Read the Denial Letter Carefully: Start by taking a moment to truly understand the reasons behind the denial. Common issues often include claims of lack of medical necessity or not meeting specific criteria outlined in your policy. It’s important to note that 64% of patients with obesity and 32% of those with type 2 diabetes have faced prescription denials for GLP-1 medications, highlighting the need for information on how to get GLP-1 covered by insurance. Additionally, 54% of GLP1Ra prescriptions for individuals with type 2 diabetes were rejected by private providers, highlighting the challenges many face in securing the support they need.
-
Review Your Insurance Policy: Take the time to examine your policy closely to determine if the denial aligns with the coverage terms. This step is crucial in identifying whether the denial was justified or if there’s a valid basis for an appeal. Many insurance firms may reject claims based on the belief that weight-loss treatments lack adequate clinical justification, but understanding your policy can empower you.
-
Gather Supporting Materials: Compile any additional records that can bolster your case, such as letters from your healthcare provider detailing the medical necessity of the medication. Insurers often require thorough documentation to justify coverage, so it’s vital that your provider highlights the clinical advantages and health results linked to the treatment. Gathering comprehensive records can significantly influence the success of your appeal, so don’t hesitate to ask for help.
-
File an Appeal: When you’re ready, draft a formal appeal letter to your provider, including all relevant information and supporting documentation. Make sure to follow the specific appeal procedure detailed in your coverage policy. If your initial appeal is denied, remember that you can request a review by an independent review organization (IRO). An IRO is an external entity that evaluates the appeal, providing an additional layer of scrutiny to the decision and advocating for your needs.
-
Follow Up: After submitting your appeal, keep the lines of communication open with your provider to confirm that it is being processed. Maintain meticulous records of all interactions, as this can be vital if further action is needed. Advocacy efforts are crucial, especially as denial rates for weight-loss treatments have risen; 60% of medical group leaders have reported higher denial rates in 2024 compared to the previous year. Furthermore, be mindful that administrative errors, such as duplicate billing or incorrect codes, can also lead to claim denials, so take a moment to double-check all submitted information. Remember, you are not alone in this journey, and together, we can navigate these challenges.
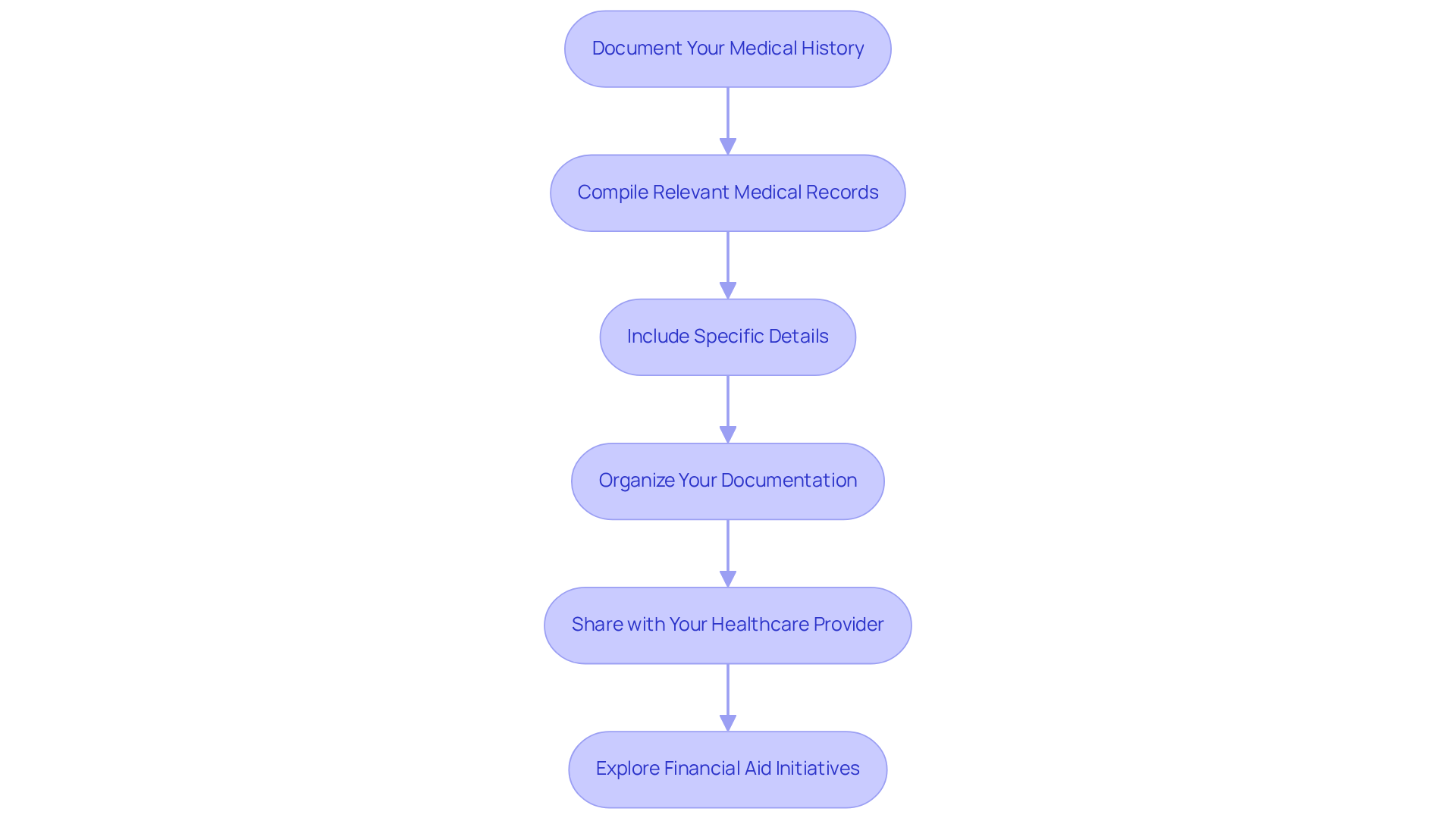
Document Your Medical History Effectively
To successfully learn how to get GLP-1 covered by insurance, it’s vital to compile and document your medical history effectively. Navigating this process can feel overwhelming, but together, we can take the necessary steps to ensure your documentation supports your prior authorization request.
-
Compile Relevant Medical Records: Start by gathering all pertinent medical records. This includes previous diagnoses, treatment plans, and details of any weight management programs you have participated in, such as those offered by Minimal. This foundational information is crucial for demonstrating medical necessity and can help you feel more prepared.
-
Include Specific Details: Document your weight history meticulously. Note any significant weight loss or gain, along with related health issues such as diabetes, hypertension, or high cholesterol. Thorough records of these factors can greatly enhance your argument for treatment approval, especially when paired with the customized fitness and nutrition plans offered by Minimal. Reflecting on your journey can empower you as you advocate for your health.
-
Organize Your Documentation: Create a well-structured file of your medical history. Include dates of visits, names of healthcare providers, and any treatments or medications prescribed. Organized records not only facilitate the approval process but also enhance the credibility of your claim. Remember, clarity in your documentation can make a significant difference.
-
Share with Your Healthcare Provider: Provide this organized record to your healthcare provider. This collaboration is vital as it assists them in submitting the prior authorization request and supports any appeals if necessary. Regular follow-ups and thorough documentation can lead to a higher success rate in obtaining approvals. Many patients secure coverage after one or two attempts, particularly when their medical history is well-documented. You are not alone in this journey.
-
Explore Financial Aid Initiatives: If your coverage does not include GLP-1 treatments, consider looking into financial aid initiatives provided by pharmaceutical companies or payment options from pharmacies. This can help reduce out-of-pocket costs and provide additional support for your weight management journey, especially through the holistic and personalized care offered by Minimal.
By following these steps, you can learn how to get GLP-1 covered by insurance, thereby enhancing your likelihood of obtaining these treatments. Remember, we’re here for you, and together, we can achieve your goals for a healthier future.
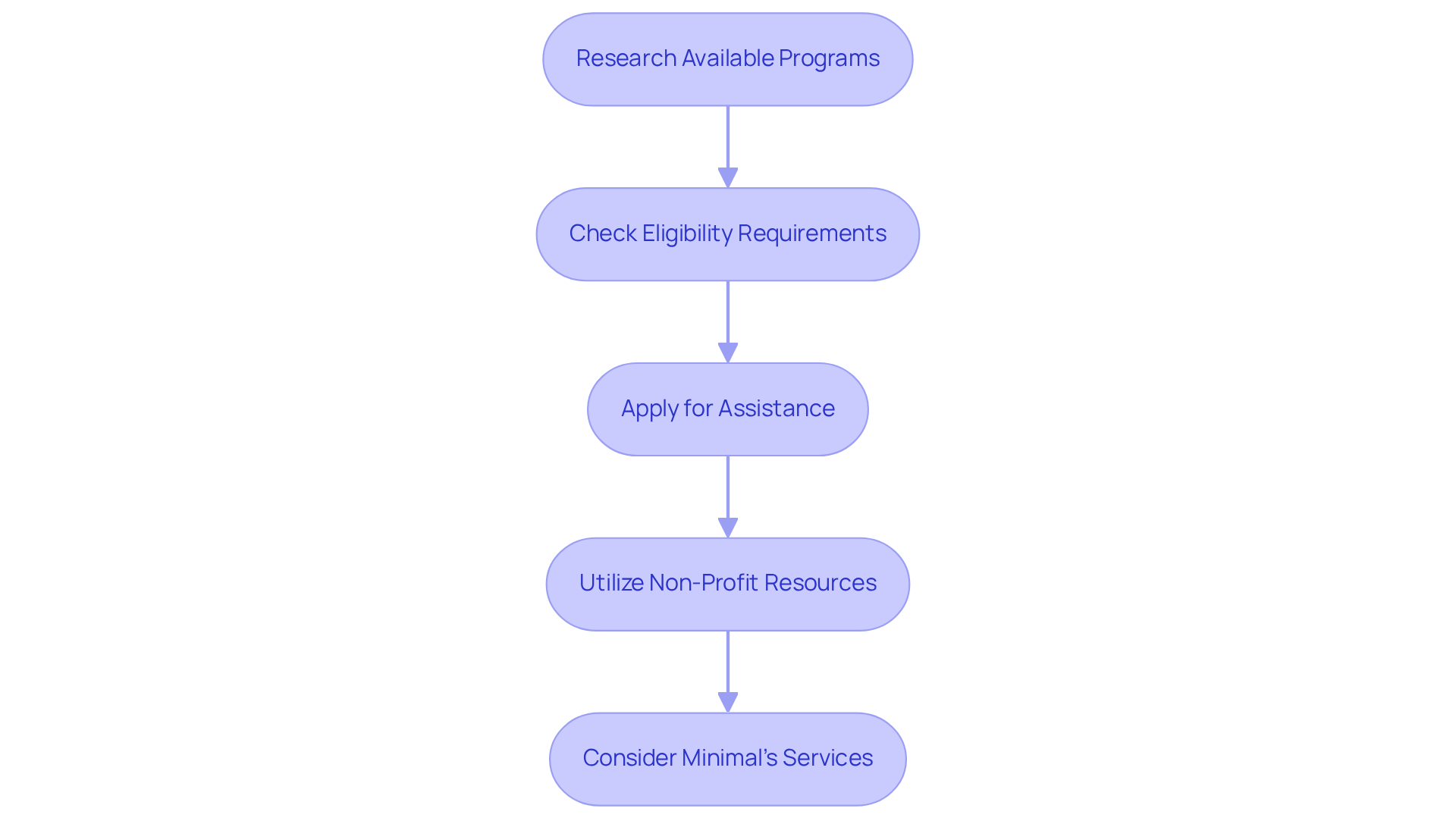
Explore Financial Assistance Programs
Investigating financial aid programs can significantly ease the financial strain of GLP-1 treatments like Ozempic® and Wegovy®. Here are some important steps to help you access these valuable resources:
-
Research Available Programs: Begin by exploring patient assistance programs offered by pharmaceutical companies. For example, Novo Nordisk provides a Patient Assistance Program specifically for Ozempic® and Wegovy®, which can help eligible patients obtain these medications at reduced or no cost.
-
Check Eligibility Requirements: Each assistance program has specific eligibility criteria, often based on income levels or insurance status. It’s essential to review these requirements carefully to see if you qualify for financial aid.
-
Apply for Assistance: After identifying programs for which you qualify, proceed with the application process. This usually involves submitting documentation related to your income and medical history. Be sure to provide all necessary information to support your application effectively.
-
Utilize Non-Profit Resources: In addition to pharmaceutical programs, consider looking into non-profit organizations that offer financial assistance for obesity treatments. Many of these organizations provide grants or funding opportunities to help cover prescription costs, making it easier for you to access the treatments you need.
-
Consider Minimal’s Services: At Minimal, we are committed to providing affordable health and wellness solutions, including free delivery right to your doorstep. With flexible pricing starting as low as $49 for the first month, we strive to make effective weight loss solutions like Ozempic® and Wegovy more accessible. By utilizing our services, you can take proactive steps toward acquiring the treatments that are essential for your health goals.
Statistics reveal that 24% of adults reported challenges affording their prescriptions in 2019, underscoring the importance of these financial assistance programs. For instance, many individuals have successfully navigated the Novo Nordisk Patient Assistance Program, with a total savings of $187,789 reported for 18 patients utilizing Medication Assistance Programs (MAP). By leveraging these resources, you can take meaningful steps toward obtaining the medications necessary for your health aspirations.
Conclusion
Navigating the complexities of insurance coverage for GLP-1 medications can feel overwhelming. We understand that individuals seeking effective weight management solutions may encounter numerous hurdles. However, by grasping the intricacies of your insurance policy and taking proactive steps, you can secure the support needed for treatments like Ozempic® and Wegovy®. It may seem daunting, but with the right information and resources, achieving coverage is absolutely within reach.
Key strategies to consider include:
- Thoroughly reviewing your insurance policy
- Understanding prior authorization requirements
- Effectively managing any denials
- Documenting your medical history meticulously
- Exploring financial assistance programs
Each of these steps plays a crucial role in preparing you to advocate for your health and access the treatments you need.
Ultimately, the pursuit of GLP-1 medications should not be hindered by insurance challenges. By leveraging these strategies and seeking assistance when necessary, you can overcome obstacles and take charge of your health journey. Embracing these steps not only empowers you but also contributes to a broader movement toward better access to essential healthcare treatments. Together, we can achieve your goals and ensure that you receive the support you deserve.
Frequently Asked Questions
How can I assess my insurance coverage for GLP-1 medications?
Start by reviewing your policy documents to find the section on prescription drug coverage, which usually includes a formulary list of covered drugs. If you have questions, contact your insurance provider using the customer service number on your card.
What should I ask my insurance provider regarding GLP-1 medications?
Inquire specifically about coverage for GLP-1 medications like Ozempic® and Wegovy®, and clarify whether they are covered for weight management or strictly for diabetes treatment.
Are there specific requirements for insurance coverage of GLP-1 medications?
Yes, many insurance plans have specific criteria, which may include a documented history of obesity or related health conditions. It’s important to ask about these requirements during your call.
Why is it important to document my findings when dealing with insurance?
Keeping a thorough record of your discussions and any written correspondence can be invaluable if you need to appeal a denial or clarify policy details later on.
What percentage of firms provide coverage for anti-obesity treatments?
Currently, around 50 million adult Americans have insurance for anti-obesity treatments, but only a small portion of large firms support GLP-1 drugs. Approximately 79% of firms that offer weight loss medications require insured members to meet specific conditions for approval.
What are prior authorization requirements for GLP-1 treatments?
Prior authorization may be necessary for GLP-1 treatments. Check with your coverage provider for specific requirements, which can typically be found in your insurance policy or formulary.
What documentation is needed for prior authorization?
Gather medical records that demonstrate the medical necessity of the medication, including your Body Mass Index (BMI), weight history, and records of previous weight management treatments.
Who submits the prior authorization request for GLP-1 medications?
Your healthcare provider usually needs to submit the prior authorization request on your behalf, including all required documentation.
How long does it typically take to process a prior authorization request?
Processing times for prior authorization requests usually range from 5 to 10 business days.
What should I do after submitting my prior authorization request?
It’s important to follow up with your insurance company to check the status of your request.
What is the significance of thorough documentation in the prior authorization process?
Many denials can be overturned on appeal with stronger documentation, highlighting the importance of thorough preparation and communication between patients and healthcare providers.