Overview
Navigating health insurance coverage can be overwhelming, especially when it comes to medications like Ozempic, which is primarily approved for type 2 diabetes. It’s important to know that Aetna’s coverage may not extend to weight loss, as many plans specifically exclude weight loss medications. This can be frustrating, but you’re not alone in this journey.
Understanding your individual plan details is crucial. Take the time to review your coverage and consider obtaining prior authorization. This process typically requires demonstrating a certain BMI or weight-related health issues, which can feel daunting. However, this step is essential to determine your eligibility for coverage.
Remember, we’re here for you. Together, we can achieve your goals, and taking these steps can help you feel more empowered in your health journey. Don’t hesitate to reach out for support as you navigate these complexities. Your health and well-being are worth it.
Introduction
Navigating the intricate landscape of health insurance can feel overwhelming, especially when trying to understand coverage for specific medications like Ozempic. This medication, primarily used for managing type 2 diabetes, has also gained attention for its off-label use in weight loss. However, Aetna’s coverage policies can present a complex web of guidelines that may leave you feeling lost. How do you determine your eligibility? From prior authorization requirements to demonstrating medical need, understanding Aetna’s criteria is essential for anyone considering this treatment.
With so much at stake and the potential for significant financial implications, being informed about your insurance plan can truly make a difference in accessing the medications you need. Remember, you’re not alone in this journey. Together, we can achieve your health goals, and being knowledgeable about your options is the first step toward empowerment. Let’s untangle these complexities together, ensuring you have the support and information necessary to move forward confidently.
Understand Aetna’s Coverage Policies for Ozempic
Navigating Aetna’s insurance policies for prescription medications can feel overwhelming, but understanding their general guidelines can help you on your journey. Aetna typically covers FDA-approved drugs for specific medical conditions, leading to inquiries about whether Aetna covers Ozempic for weight loss, since it is primarily authorized for managing type 2 diabetes and is often recommended off-label for reducing body mass. However, it’s important to note that many Aetna plans specifically omit benefits for weight loss medications, leading to the inquiry: does Aetna cover Ozempic for weight loss? To find the specific exclusions and criteria that may apply to your situation, we encourage you to refer to the Aetna Drug Guide and relevant policy documents. You can access these resources on Aetna’s official site or reach out to their customer service for detailed information tailored to your plan’s benefits.
Did you know that recent statistics show roughly two-thirds of self-funded plan sponsors incorporate GLP-1 medications like Ozempic in their anti-obesity support? While this is promising, a July 2023 report revealed that about two-thirds of patients stop using medications for reducing body mass within a year, even when insurance covers them. In California, for instance, benefits for appetite suppressant medications vary by plan, with some requiring prior approval and proof of medical necessity for benefits. This variability underscores the importance of understanding your specific plan’s provisions regarding Ozempic and other treatments for reducing body mass, particularly whether Aetna covers Ozempic for weight loss. As comedian Amy Schumer aptly pointed out, navigating insurance options can be challenging. However, being informed is key to accessing the treatments you need. Additionally, if you’re enrolled in Level Funded plans with Cigna, you may have the option to choose benefits for appetite suppressants at a higher expense, showcasing the various choices available based on your plan. Remember, you’re not alone in this journey; together, we can achieve your goals.
Does Aetna Cover Wegovy for Weight Loss?
If you’re exploring GLP-1 medications for weight loss, you may be wondering whether Aetna covers Wegovy. Unlike Ozempic, which is approved for type 2 diabetes, Wegovy uses the same active ingredient—semaglutide—but is FDA-approved specifically for chronic weight management.
Aetna may offer clearer coverage pathways for Wegovy than for Ozempic, but eligibility still depends on your plan details and health status. Most plans that cover Wegovy require:
-
A body mass index (BMI) of 30 or higher, or
-
A BMI of 27 or higher with a weight-related condition such as hypertension or type 2 diabetes
Just like with any GLP-1 medication, Aetna may also ask for prior authorization, medical documentation, or proof that other weight loss treatments were attempted first.
If Wegovy is unavailable—due to supply shortages or formulary exclusions—some Aetna plans might consider alternatives or allow off-label use of other medications like Ozempic.
To avoid surprises, it’s best to check your plan’s drug formulary, speak with an Aetna representative, and work with your healthcare provider to gather the necessary documentation. Knowing what your policy includes can help you make informed decisions and reduce unexpected out-of-pocket costs.
Review Aetna’s Criteria for Ozempic Coverage
The question of whether Aetna covers Ozempic for weight loss is influenced by several factors, including your medical history and diagnosis. If you’re considering whether Aetna covers Ozempic for weight loss rather than diabetes treatment, prior approval is typically necessary. To determine if Aetna covers Ozempic for weight loss, you generally need to show a body mass index (BMI) of 30 or higher, or a BMI of 27 or greater accompanied by weight-related health issues. It’s often crucial to provide records from your healthcare professionals that detail your weight loss history and previous treatment attempts.
Ozempic, a GLP-1 medication, is FDA-approved for managing type 2 diabetes and has shown significant benefits in weight management. It helps regulate blood sugar levels and can lower the risk of heart problems, making it an important option for those with diabetes who are looking to lose weight. It’s noteworthy that 90-95% of individuals with diabetes in the U.S. have type 2 diabetes, highlighting how essential this medication is for addressing weight loss, especially within this group. Aetna’s Clinical Policy Bulletins outline specific criteria for coverage, including whether Aetna covers Ozempic for weight loss, which can vary based on individual circumstances. Continuous treatment is vital to maintain progress in weight and health, as researchers emphasize the importance of a comprehensive approach to weight management.
When using Ozempic, it is usually administered weekly, with or without food, via a pre-filled pen. You should inject it into your stomach, thigh, or upper arm, always using a new needle for each injection and storing the pen according to the instructions provided. It’s important to follow your doctor’s dosing guidelines closely, especially when considering if Aetna covers Ozempic for weight loss, to ensure safe and effective use. If you have a history of pancreatitis or type 1 diabetes, please exercise caution, as the safety and effectiveness of this medication for these populations have not been established.
Real-life stories illustrate how Aetna’s criteria are applied, emphasizing the need for thorough documentation and adherence to medical necessity standards. We encourage you to consult with your healthcare provider to ensure all necessary information is ready for submission, helping to make the authorization process smoother. Additionally, since this medication can be expensive for those without prescription insurance, it’s wise to explore Novo Nordisk’s patient assistance programs and savings cards, which can significantly ease the financial burden for eligible individuals. Lastly, it’s crucial to check your insurance plan’s drug formulary for coverage details on this medication, ensuring you are well-informed about your options. Together, we can navigate this journey towards better health.
For added perspective, Ozempic’s list price without insurance is currently around $1,351 for a one-month supply (four single-dose pens), totaling more than $16,000 per year. With insurance, out-of-pocket costs depend on your plan’s formulary tier. As a brand-name drug, Ozempic is often categorized as tier two or higher, where copays generally range from $36 to $65—but they can be higher depending on your policy. Prices may also vary based on your pharmacy and location.
By understanding these pricing factors and exploring available resources—like discount programs, pharmacy comparisons, or patient assistance through Novo Nordisk—you can take meaningful steps toward making your treatment more affordable.
Additional Ways to Save on Ozempic Without Insurance
Ozempic can be expensive for those without prescription coverage, but there are practical steps you can take to reduce your out-of-pocket costs:
-
Compare pharmacy prices: Drug costs can vary significantly depending on the pharmacy and location. Check prices online or call local pharmacies to find the most affordable option in your area.
-
Use pharmacy discount programs: Savings tools like GoodRx or SingleCare can lower the cash price by hundreds of dollars, making Ozempic more accessible.
-
Check eligibility for manufacturer savings: Novo Nordisk offers savings cards and patient assistance programs for eligible individuals, which may help offset the cost of Ozempic.
-
Explore other insurance options: If your current insurance plan doesn’t cover Ozempic, consider switching to one that does during Open Enrollment or after a qualifying life event like a move or job change.
Always verify pricing and eligibility details with your pharmacist and insurance provider, and avoid purchasing from unauthorized sources offering suspiciously low prices. Staying informed helps protect both your wallet and your health.
Alternatives Aetna May Require Before Approving Ozempic
Before approving Ozempic, Aetna may require you to go through a “step therapy” process. This means trying other, often more affordable or established, type 2 diabetes medications first. Common alternatives include generic drugs like metformin or medications such as Victoza (liraglutide), which have been widely prescribed for blood sugar management.
If these initial medications prove ineffective or cause unwanted side effects, your healthcare provider can document those experiences in a prior authorization request. This documentation plays a key role in demonstrating medical necessity, especially when requesting a newer treatment like Ozempic or Mounjaro.
Working closely with your doctor ensures your medical history is properly recorded and submitted to Aetna. This can make the approval process smoother and improve your chances of getting coverage for the medication that best fits your health needs.
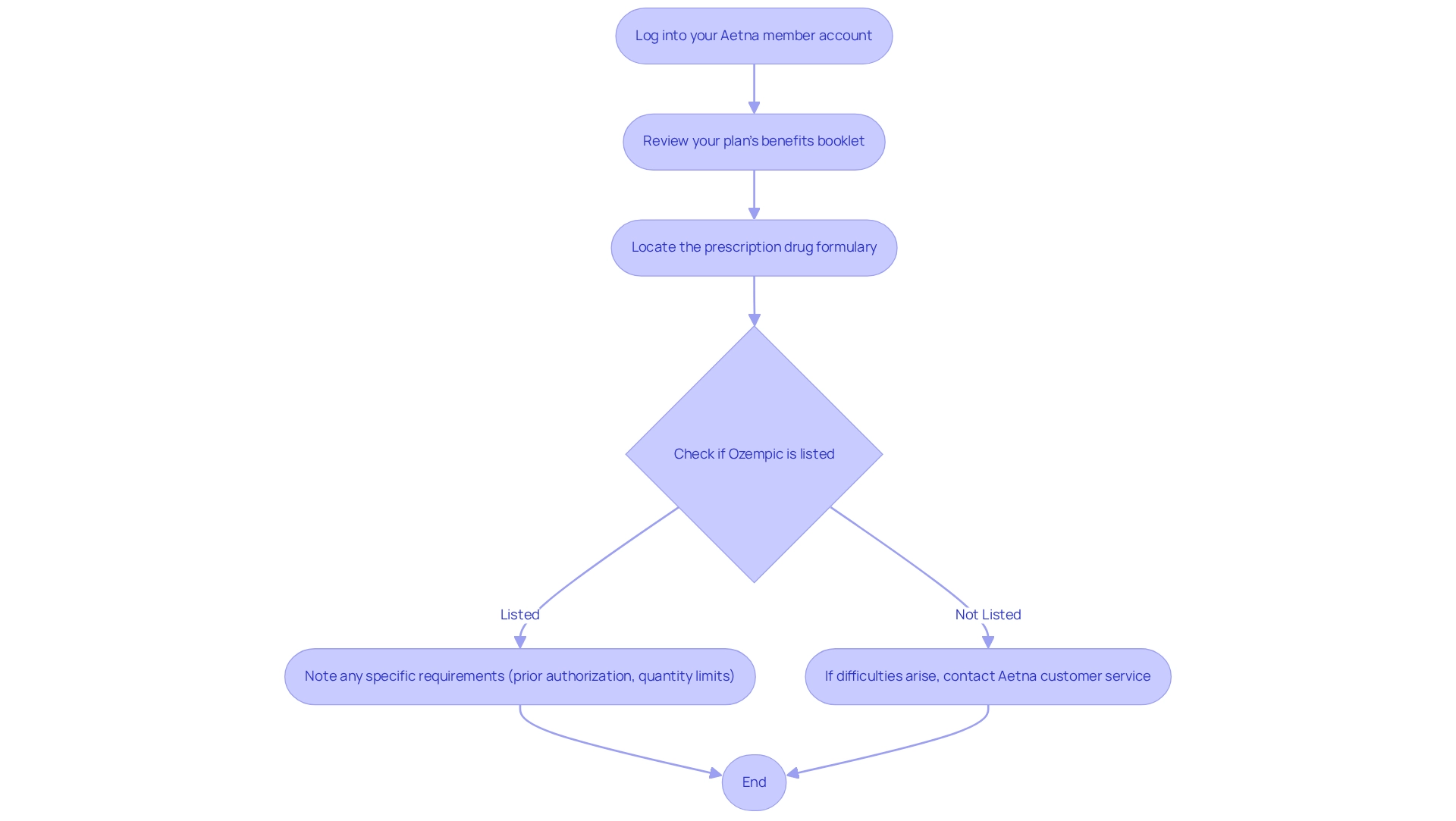
Check Your Aetna Plan Details for Ozempic Coverage
To determine if your Aetna plan includes the medication, we encourage you to start by logging into your Aetna member account online or reviewing your plan’s benefits booklet. Within these resources, you can locate the prescription drug formulary, which details the medications covered under your plan. If you find the medication listed, please pay attention to any specific requirements, such as prior authorization or quantity limits that may apply.
Ozempic, a GLP-1 drug, assists in lowering blood sugar levels in type 2 diabetes and encourages a reduction in appetite. This makes it a valuable choice for those seeking effective management solutions. It’s important to investigate if Aetna covers Ozempic for weight loss before consulting your doctor. Doing so can save you time and ensure you have the necessary information at hand.
Should you encounter difficulties finding this information online, don’t hesitate to reach out to Aetna’s customer service using the number provided on your member ID card. Their representatives are here to provide tailored support and address any inquiries regarding your benefits, ensuring you have the essential information to make informed choices about your treatment options.
Remember, comprehending your benefits is crucial. Curex has transformed the lives of over 300,000 patients by offering accessible treatment options. As Ana C. noted, ‘The Curex staff has been professional, efficient, and really focused on my individual needs.’ This highlights the importance of having a supportive team when navigating your health journey. Together, we can achieve your goals, and we’re here for you every step of the way.
How Much Could Ozempic Cost with Aetna Insurance?
The cost of Ozempic with Aetna insurance can vary, but it’s important to understand the potential out-of-pocket expenses before starting treatment. Without insurance, a one-month supply of Ozempic may cost over $1,300, making coverage a major factor in affordability.
With Aetna, Ozempic is typically classified as a brand-name drug—often in tier two or higher. That means you won’t pay the full price, but your copay or coinsurance will depend on your plan’s drug formulary.
Here are a few things to consider when estimating your cost:
-
Tier placement: If Ozempic is in a higher tier, your cost share may be higher.
-
Copay or coinsurance: These amounts vary by plan, but national averages show copays for tier two and three medications range from about $36 to $65.
-
Pharmacy differences: Prices may change depending on where you fill your prescription.
If cost is a concern, ask your provider about manufacturer savings programs or patient assistance options. You may also want to contact Aetna directly or review your member portal for plan-specific pricing details. A little research upfront can help avoid unexpected expenses and ensure you get the support you need.
Explore Options If Aetna Denies Ozempic Coverage
If Aetna denies coverage for your medication, remember that you have the right to appeal this decision. Start by carefully reviewing the denial letter to understand the specific reasons behind it. Then, gather supporting documentation from your healthcare provider, which should include medical records and a detailed letter of medical necessity explaining why this medication is essential for your treatment.
This GLP-1 medication is designed to help lower blood sugar levels in type 2 diabetes and promote a decrease in appetite. Administered once a week via injection into the stomach, thigh, or upper arm, your doctor will guide you on how to use the pre-filled pen. Always use a new needle for each injection and store the pen as directed to ensure safe and effective use. It’s important to note that Ozempic’s safety and effectiveness have not been confirmed for individuals with a history of pancreatitis or type 1 diabetes.
When you’re ready to submit your appeal, you can do so through Aetna’s member services, either online or via mail. Just be sure to adhere to any specified deadlines. Following up on the status of your appeal regularly is crucial, and be prepared to provide additional information if requested.
Statistics show that among Covered California insurers, approximately 40% of internal appeals filed were upheld. This highlights the potential for success in challenging denials. Furthermore, a recent case study revealed that 55% of respondents believe regulating insurers’ claims decisions should be a top priority for Congress. This growing public concern may empower you in your appeal process.
If your appeal is unsuccessful, consider discussing alternative medications with your healthcare provider or exploring patient assistance programs offered by the manufacturer. Dr. Chance Miller emphasizes that clients appreciate the personalized attention from a dedicated care team, which can be invaluable during this challenging time. This proactive approach can help you navigate the complexities of insurance coverage, particularly when asking does Aetna cover Ozempic for weight loss, and find the support you need on your journey. Remember, together, we can achieve your goals.
Conclusion
Understanding Aetna’s coverage policies for medications like Ozempic is essential for anyone seeking effective treatment for type 2 diabetes and weight management. We know that the complexities of insurance coverage can feel overwhelming, especially when it comes to criteria such as prior authorization and medical necessity. By familiarizing yourself with Aetna’s guidelines, including the need for documentation and specific health requirements, you can better navigate your options and improve your chances of obtaining coverage.
If your coverage is denied, remember that taking action is crucial. Appeal the decision with the appropriate documentation from your healthcare providers. This process may involve gathering medical records and providing a detailed explanation of why Ozempic is necessary for your treatment. With a significant number of appeals being upheld, there is a pathway to challenge denials, reinforcing the importance of persistence and thoroughness in pursuing the care you need.
Ultimately, being proactive and informed about insurance plans empowers you and enhances your ability to access necessary medications. The journey to effective health management can be complex, but with the right knowledge and support, together we can overcome obstacles and achieve your health goals confidently. Remember, you are not alone in this journey—we’re here for you every step of the way.
Frequently Asked Questions
What does Aetna typically cover regarding prescription medications?
Aetna typically covers FDA-approved drugs for specific medical conditions.
Does Aetna cover Ozempic for weight loss?
Many Aetna plans specifically omit benefits for weight loss medications, so coverage for Ozempic for weight loss may not be available.
How can I find out if my Aetna plan covers Ozempic?
To find the specific exclusions and criteria that may apply to your situation, refer to the Aetna Drug Guide and relevant policy documents, which can be accessed on Aetna’s official site or by contacting their customer service.
What recent statistics are there regarding the use of GLP-1 medications like Ozempic?
Recent statistics show that roughly two-thirds of self-funded plan sponsors incorporate GLP-1 medications like Ozempic in their anti-obesity support.
What challenges do patients face when using medications for weight loss?
A July 2023 report revealed that about two-thirds of patients stop using medications for reducing body mass within a year, even when insurance covers them.
How do benefits for appetite suppressant medications vary in California?
In California, benefits for appetite suppressant medications vary by plan, with some requiring prior approval and proof of medical necessity for benefits.
What options might I have if enrolled in Level Funded plans with Cigna?
If you’re enrolled in Level Funded plans with Cigna, you may have the option to choose benefits for appetite suppressants at a higher expense, showcasing the various choices available based on your plan.
How much does Ozempic cost without insurance?
Without insurance, a one-month supply of Ozempic typically costs around $1,350, totaling over $16,000 per year. These high out-of-pocket costs make it important to explore manufacturer savings programs or talk to your healthcare provider about alternatives.
How can I avoid counterfeit Ozempic?
To protect your health, always fill your Ozempic prescription at a licensed pharmacy and avoid suspiciously low-priced offers or unverified online sources. Speak with your doctor about savings programs from Novo Nordisk to reduce costs safely without compromising on authenticity.
Should I be worried about counterfeit or compounded Ozempic?
Yes. Both the World Health Organization and the FDA have issued warnings about counterfeit Ozempic in the supply chain, which may contain harmful or ineffective ingredients. Additionally, compounded semaglutide—often advertised as “generic Ozempic”—lacks FDA approval and carries risks like incorrect dosing or contamination. To stay safe, only purchase Ozempic from licensed pharmacies and speak with your doctor about official savings programs.