Overview
Navigating the insurance process for Semaglutide can feel daunting, but we’re here to help you every step of the way. To start, gather the necessary documentation that will support your case. Next, reach out to your insurance provider to inquire about coverage options. It’s important to be prepared to appeal any denied claims, as this can make a significant difference in your journey.
Consider collecting your medical records and prescription information. What questions do you have for your insurance provider? Preparing these in advance can empower you during your discussions. Understanding the appeal process is also crucial; it can significantly enhance your chances of securing coverage for this effective weight loss treatment.
Remember, you are not alone in this process. Together, we can achieve your goals and ensure that you receive the support you need. Take these steps with confidence, and know that each action brings you closer to your weight loss journey.
Introduction
Navigating the complexities of health insurance can feel overwhelming, especially when it comes to securing coverage for essential medications like Semaglutide, a powerful ally in the fight against obesity. This guide is designed to illuminate the pathway for individuals seeking to understand how to get Semaglutide covered by insurance, ensuring access to its remarkable benefits for weight loss.
However, this journey often raises important questions:
- What documentation is necessary?
- How can you effectively appeal a denied claim?
As you explore this step-by-step guide, you’ll discover the strategies needed to overcome these challenges and take control of your health journey. Remember, you’re not alone in this; together, we can navigate these hurdles and achieve your goals.
Understand Semaglutide and Its Benefits for Weight Loss
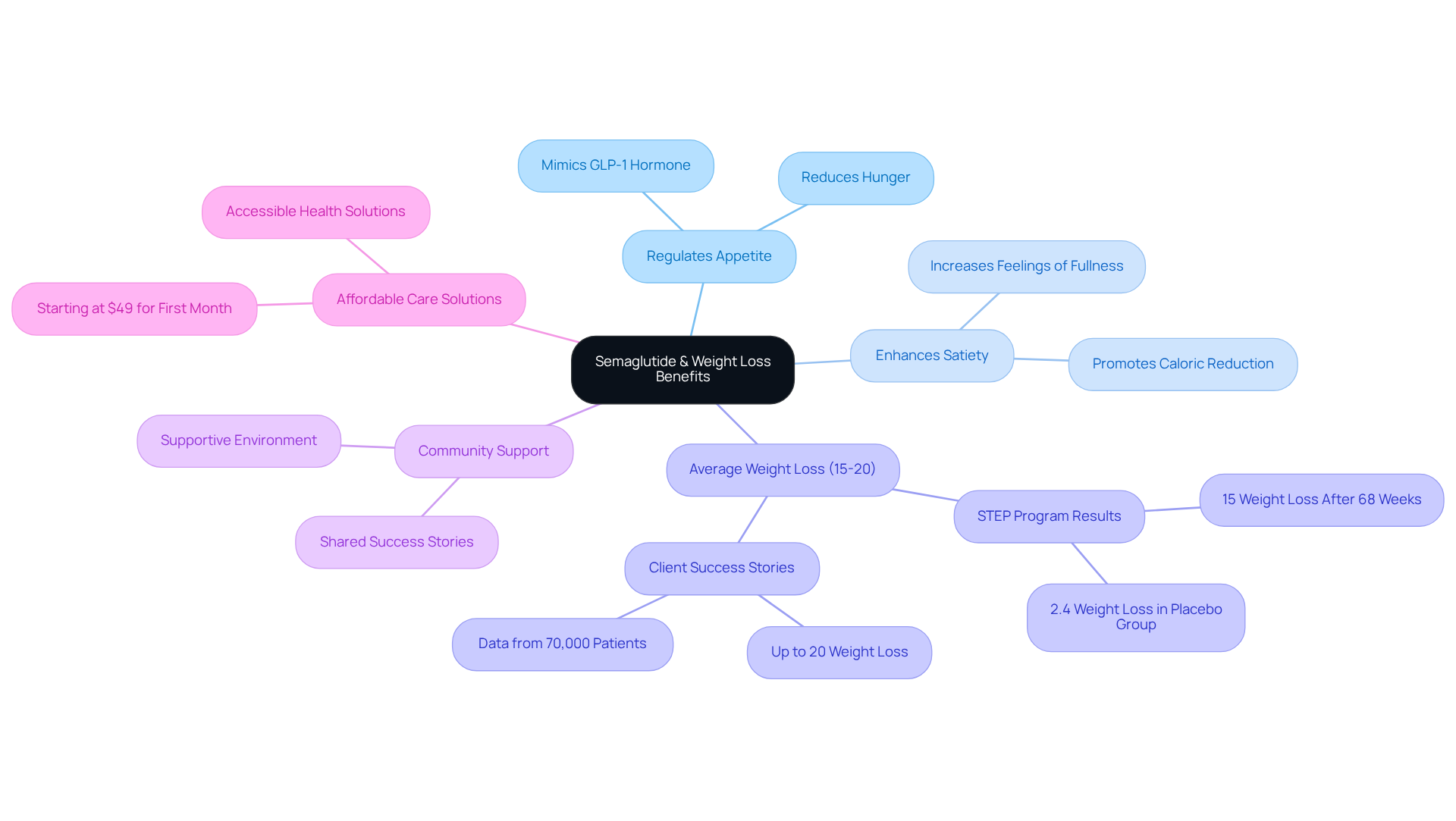
The GLP-1 receptor agonist is a valuable ally in your weight loss journey, playing a crucial role in reducing body mass by regulating appetite and enhancing satiety. By mimicking the hormone GLP-1, it positively influences glucose metabolism and appetite control.
Imagine being part of a community where individuals using Semaglutide can achieve an impressive average reduction of 15-20% of their body mass, especially when combined with supportive lifestyle changes. For instance, participants in the STEP program experienced an average loss of 15% of their initial body mass after just 68 weeks of treatment.
This remarkable decrease not only helps you reach your personal health objectives but also provides a compelling reason to understand how to get semaglutide covered by insurance. It can motivate you to embrace this effective therapy as part of your transformative journey.
Many customers have shared their inspiring success stories, highlighting how Minimal’s comprehensive care and support have positively impacted their lives. With services starting at just $49 for the first month, Minimal offers an affordable choice for those seeking tailored health solutions and a holistic approach to weight loss.
Remember, we’re here for you, and together, we can achieve your goals.
Gather Necessary Documentation for Insurance Coverage
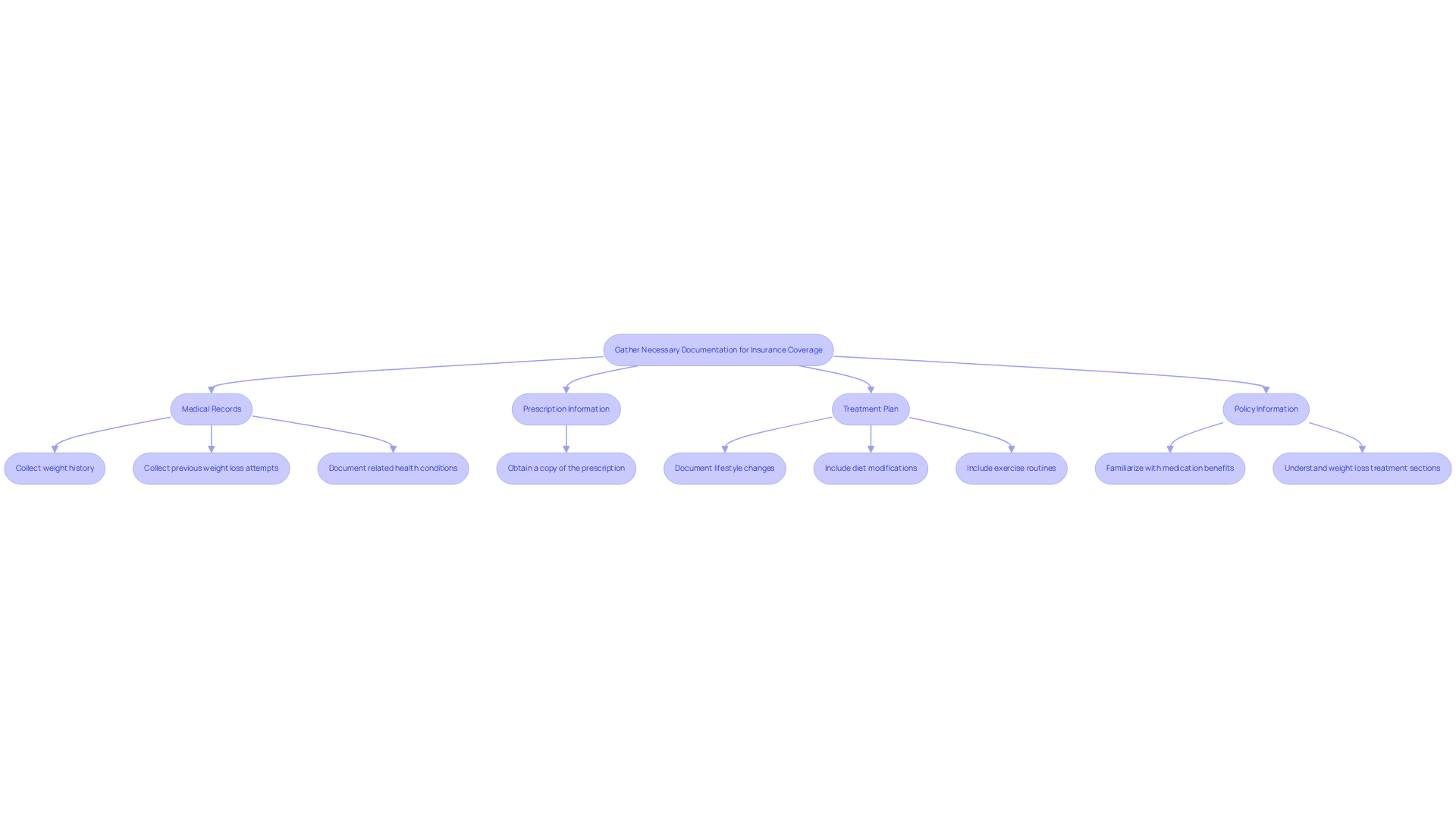
To effectively learn how to get semaglutide covered by insurance, it’s essential to gather specific documentation that demonstrates medical necessity and supports your weight loss journey. Here are some items you may need:
- Medical Records: Collect comprehensive records from your healthcare provider that detail your weight history, previous weight loss attempts, and any related health conditions, such as diabetes or hypertension. This information is vital, as insurance companies often require evidence of medical necessity.
- Prescription Information: Make sure you have a copy of the prescription for Semaglutide issued by your healthcare provider. This document confirms that the medication is an integral part of your treatment plan.
- Treatment Plan: Document any lifestyle changes you are making, including diet modifications and exercise routines. This not only supports your weight loss efforts but also demonstrates your commitment to a holistic approach to health, which is a cornerstone of Minimal’s personalized fat loss program.
- Policy Information: Familiarize yourself with your policy, especially the sections related to medication benefits and weight loss treatments. Understanding the specifics of your plan can help you navigate the claims process more effectively.
Having these documents ready will make your engagement with your insurance provider smoother, which can help you understand how to get semaglutide covered by insurance. Many clients experience significant weight loss, with data suggesting that participants in similar programs can lose up to 20% of their body mass within six months. This highlights the potential efficacy of the medication in your weight loss journey.
If you need additional support, please connect with Minimal Support by phone at (872) 228 – 2358 or email at [email protected] for personalized consultations and assistance. Remember, understanding how to get semaglutide covered by insurance can vary based on factors like location and specific company policies. Some providers may require prior authorization for GLP-1 injections, adding complexity to the process. But together, we can navigate these challenges and work towards your goals.
Contact Your Insurance Provider to Inquire About Coverage
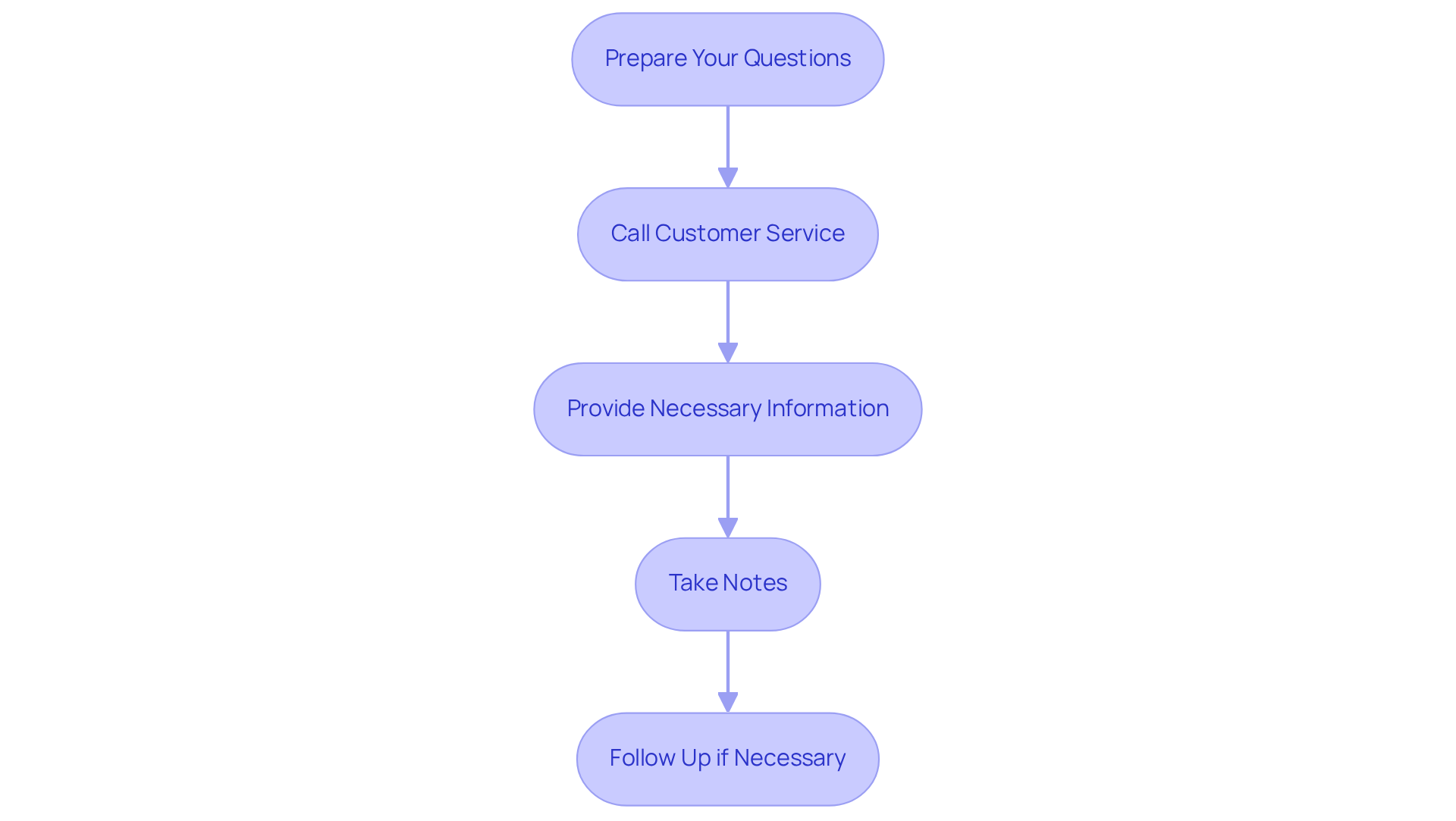
Once you’ve gathered the necessary documentation, the next step is to reach out to your insurance provider to discuss how to get semaglutide covered by insurance. Navigating this process can feel overwhelming, but we’re here to help you through it:
-
Prepare Your Questions: Before you make that call, take a moment to compile a list of specific inquiries regarding Semaglutide coverage. Consider questions like:
- Is Semaglutide covered under my plan?
- What documentation is required for approval?
- Are there any prerequisites for coverage?
-
Call the Customer Service Number: Use the number found on the back of your insurance card to connect with customer service. Keep your policy number handy for reference, as it will help streamline the conversation.
-
Provide Necessary Information: Clearly explain your situation, including relevant medical history and your reasons for seeking the medication. Don’t hesitate to mention any related health conditions that could strengthen your case for benefits.
-
Take Notes: Document the names of the representatives you speak with, their responses, and any instructions they provide. This record will be invaluable for any follow-up or appeals process.
By following these steps, you can simplify your inquiry about the medication’s support and enhance your chances of securing the essential assistance you need for your weight management journey. Remember, together, we can achieve your goals.
Appeal Denied Claims for Semaglutide Coverage
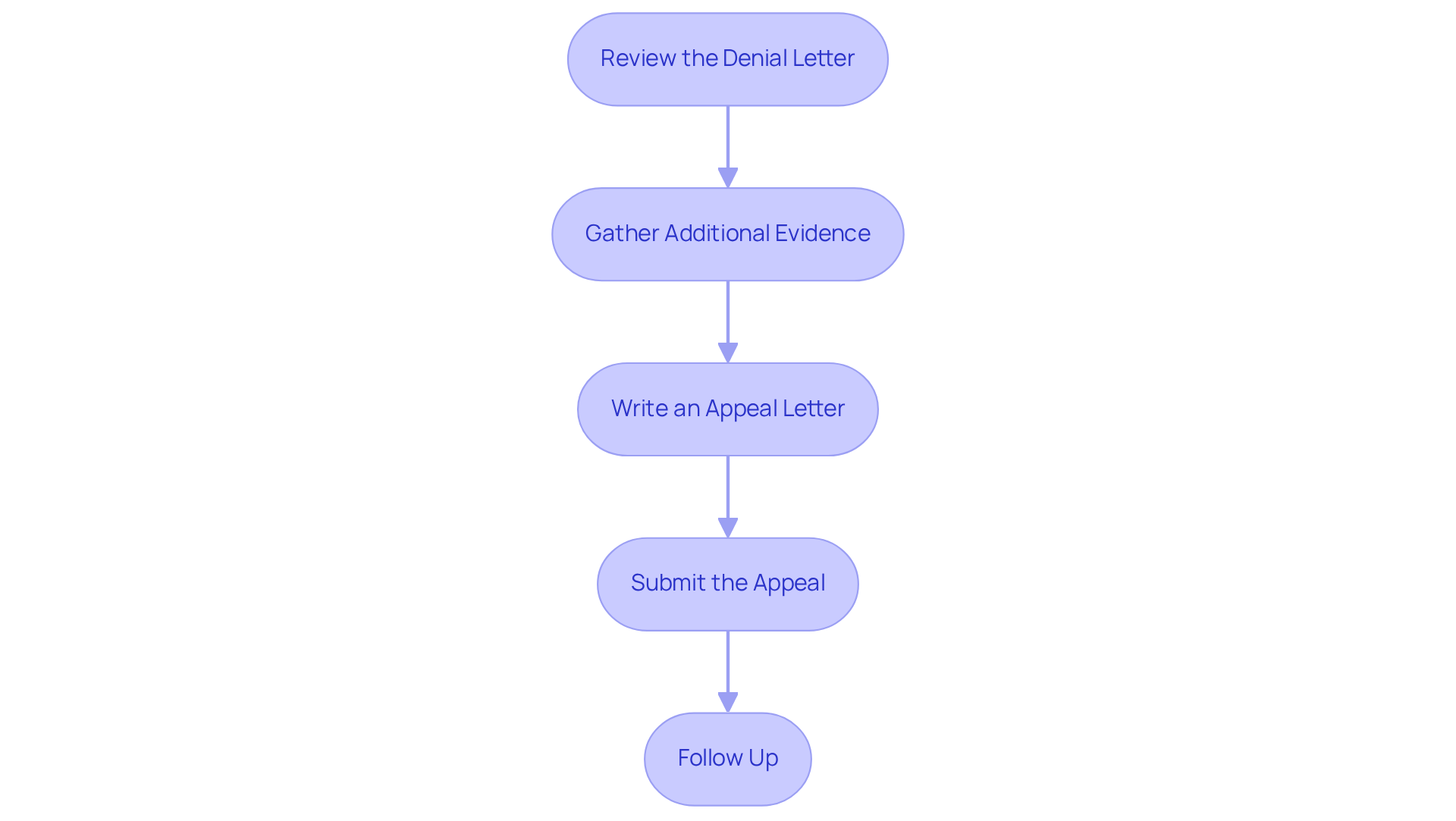
If your claim for medication coverage is rejected, don’t lose hope. You can appeal the decision by following these steps:
-
Review the Denial Letter: Take a moment to understand the reasons for the denial. Common reasons include lack of medical necessity or insufficient documentation. In fact, did you know that 8% of denials are due to lack of prior authorization, while a significant 76.5% fall under other reasons?
-
Gather Additional Evidence: If necessary, collect more documentation that supports your case, such as additional medical records or letters from your healthcare provider explaining the need for Semaglutide. Remember, comprehensive evidence is crucial for strengthening your appeal.
-
Write an Appeal Letter: Draft a formal appeal letter addressed to your provider. Include:
- Your policy number and claim details.
- A clear explanation of why you believe the denial was incorrect, referencing any relevant medical history or treatment guidelines.
- Any additional evidence you have gathered.
-
Submit the Appeal: Send your appeal letter and supporting documents to the address provided in the denial letter. Ensure you keep copies for your records. It’s important to note that coverage providers typically take 30 to 60 days to process an appeal decision.
-
Follow Up: After submitting your appeal, check back with your provider to inquire about the status of your claim. Persistence can often lead to a favorable outcome, as issuers upheld 59% of denials that were appealed by consumers. As Honest Care states, “We believe every insurance denial should be appealed and every patient should fight for access to the best treatments.”
By understanding the common reasons for Semaglutide coverage denial and employing effective appeal strategies, you can enhance your chances of securing the necessary treatment. The appeal process may take time, so remember that patience and thoroughness are essential. Together, we can navigate this journey and work towards achieving your health goals.
Conclusion
Understanding how to secure insurance coverage for semaglutide is essential for anyone embarking on a weight loss journey with this effective medication. By following these steps, you can navigate the complexities of insurance coverage, ensuring access to a treatment that has demonstrated remarkable results in reducing body mass and enhancing overall health.
Key points to consider include:
- Gathering necessary documentation, such as medical records and prescription information, to illustrate medical necessity.
- Reaching out to your insurance provider with well-prepared inquiries.
- Maintaining persistence in the face of claim denials, which are vital strategies for securing coverage.
The potential for significant weight loss, supported by various studies and success stories, highlights the value of semaglutide as part of a comprehensive weight management plan.
Ultimately, the journey to obtaining semaglutide coverage goes beyond paperwork; it is about advocating for your health and well-being. By taking proactive steps and utilizing available resources, you can overcome obstacles and access the transformative benefits of semaglutide. Embrace this process with determination, and remember, support is available to help you achieve your health goals and improve your quality of life.
Frequently Asked Questions
What is Semaglutide and how does it work for weight loss?
Semaglutide is a GLP-1 receptor agonist that helps in weight loss by regulating appetite and enhancing satiety. It mimics the hormone GLP-1, positively influencing glucose metabolism and appetite control.
What kind of weight loss can individuals expect when using Semaglutide?
Individuals using Semaglutide can achieve an average reduction of 15-20% of their body mass, especially when combined with supportive lifestyle changes.
What results did participants in the STEP program experience with Semaglutide?
Participants in the STEP program experienced an average loss of 15% of their initial body mass after just 68 weeks of treatment.
Why is it important to understand insurance coverage for Semaglutide?
Understanding how to get Semaglutide covered by insurance can motivate individuals to embrace this effective therapy as part of their weight loss journey.
What support does Minimal offer for individuals using Semaglutide?
Minimal provides comprehensive care and support, with many customers sharing inspiring success stories about how it has positively impacted their lives.
How much does it cost to start services with Minimal?
Services with Minimal start at just $49 for the first month, making it an affordable choice for those seeking tailored health solutions and a holistic approach to weight loss.