Overview
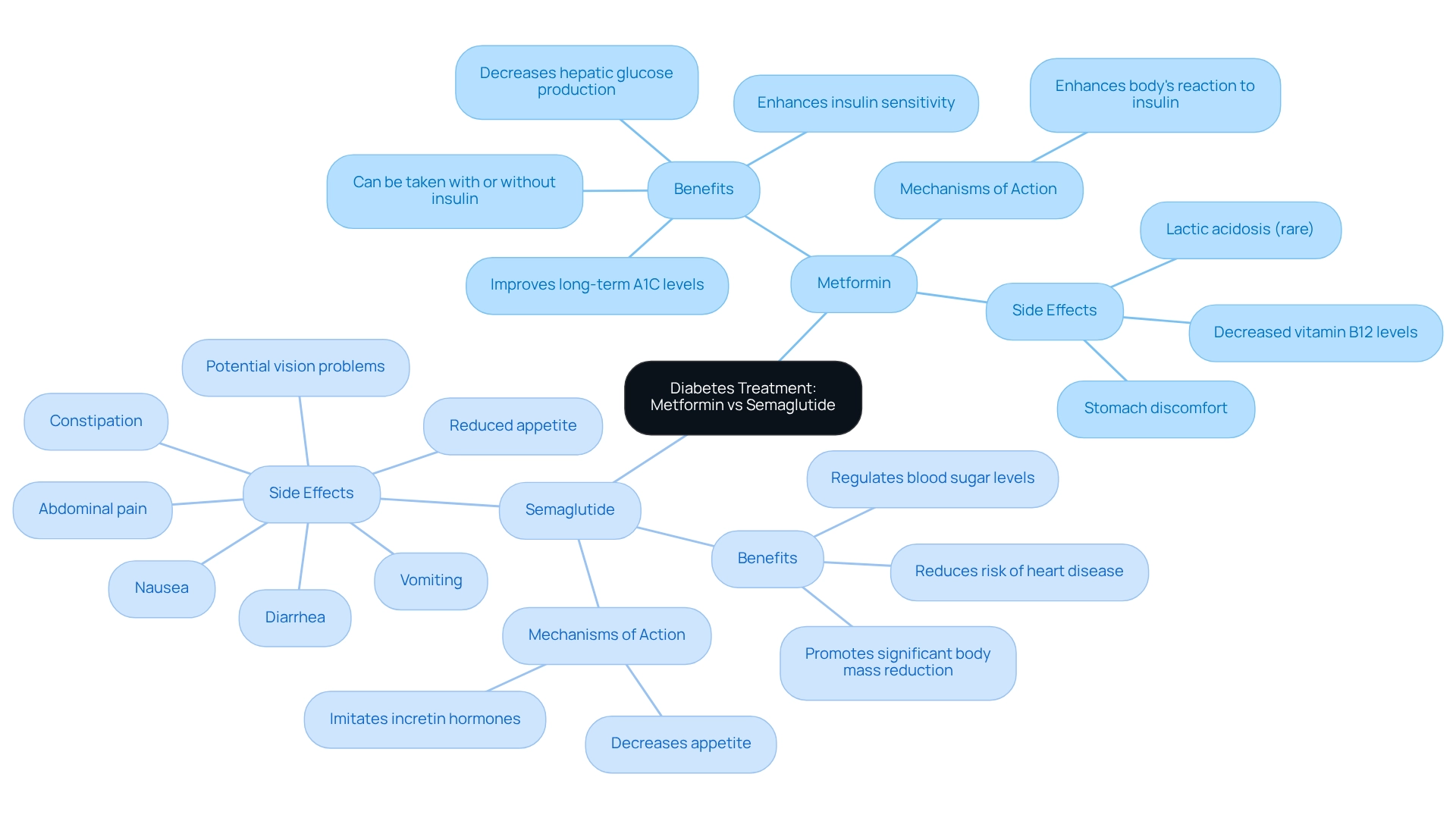
Managing type 2 diabetes can feel overwhelming, especially when it comes to choosing the right treatment. In this article, we explore the efficacy, safety, and weight loss effects of two important medications: Metformin and Semaglutide. Metformin has long been a trusted first-line treatment, known for its strong safety profile. It’s comforting to know that many have successfully managed their diabetes with it.
On the other hand, Semaglutide, a GLP-1 receptor agonist, offers additional benefits. Not only does it effectively regulate blood sugar levels, but it also promotes significant weight loss. This makes it particularly valuable for those facing obesity-related diabetes. Imagine feeling more in control of your health and weight!
We understand that every individual’s journey is unique, and finding the right solution can be challenging. Together, we can explore these options and find what works best for you. Remember, you’re not alone in this journey. We’re here for you, and with the right support, you can achieve your health goals.
Introduction
In the realm of diabetes management, we understand that the journey can feel overwhelming. However, the landscape is rapidly evolving with innovative treatments designed to meet diverse patient needs. Metformin, a long-standing staple in the fight against type 2 diabetes, continues to be celebrated for its effectiveness in enhancing insulin sensitivity and managing blood sugar levels. Meanwhile, Semaglutide has emerged as a groundbreaking option, aiding glycemic control while also promoting significant weight loss. This makes it particularly appealing for those battling obesity-related diabetes.
As healthcare providers navigate the complexities of these medications, it’s crucial to understand their distinct mechanisms, benefits, and safety profiles. This knowledge can help optimize treatment strategies and improve patient outcomes. Together, we can explore the roles of Metformin and Semaglutide, shedding light on their efficacy and the vital considerations for effective diabetes care. Remember, we’re here for you, and with the right support, you can achieve your health goals.
Overview of Metformin and Semaglutide in Diabetes Treatment
Overview of a Key Medication and an Alternative in Diabetes Treatment
Managing type 2 diabetes can feel overwhelming, but understanding your options can empower you on this journey. One key medication stands as a cornerstone in diabetes management, recognized for its ability to enhance insulin sensitivity and decrease hepatic glucose production. As a first-line treatment, it boasts a well-established efficacy and safety profile, making it a preferred choice among healthcare providers.
In contrast, a GLP-1 receptor agonist, administered via injection, offers additional benefits. Not only does it aid in blood sugar regulation, but it also facilitates significant reduction in body mass, which is particularly beneficial for patients grappling with obesity-related diabetes.
Benefits of the alternative medication:
- Lowers blood sugar levels in individuals with type 2 diabetes.
- Improves insulin sensitivity, aiding in body mass management.
- Reduces the risk of heart disease and other diabetic complications.
- Improves long-term A1C levels for better glucose control.
- Can be taken with or without insulin.
Benefits of the GLP-1 receptor agonist:
- Regulates blood sugar levels effectively.
- Promotes significant body mass reduction, with many patients reporting reductions of up to 20% when combined with lifestyle changes.
The mechanisms of action for these two medications differ markedly. The key medication primarily functions by enhancing the body’s reaction to insulin, while metformin and semaglutide work together by imitating the incretin hormones that encourage insulin release in response to meals, thus decreasing appetite and facilitating loss of body mass. Understanding these distinctions is vital in customizing treatment plans to meet your individual needs.
Recent statistics show an increasing occurrence of type 2 diabetes, with prescriptions for this medication remaining high in 2025 as healthcare providers continue to emphasize its use for initial diabetes management. Furthermore, ongoing research highlights the importance of diabetes education and lifestyle modifications to enhance treatment outcomes. Together, we can focus on these elements for successful diabetes management. Case studies have demonstrated the effectiveness of metformin and semaglutide, indicating that many patients frequently experience better glycemic control and management of their body mass. Meanwhile, the GLP-1 receptor agonist has emerged as a powerful adjunct therapy, with numerous patients reporting substantial weight loss. However, it is essential to remain vigilant regarding safety concerns, particularly its association with potential vision problems, as highlighted in an FDA data analysis. This necessitates careful monitoring of patients using the medication for potential ocular side effects. Deliana Infante notes that side effects can include nausea, vomiting, diarrhea, constipation, abdominal pain, and reduced appetite, which further underscores the need for vigilance in patient care. While this medication is generally well-tolerated, it can cause stomach discomfort, decreased vitamin B12 levels with prolonged use, and in rare instances, lactic acidosis if not utilized correctly.
In conclusion, both medications play essential roles in diabetes management, each providing distinct advantages that suit various patient profiles. By understanding their differences and applications, we can optimize treatment strategies and improve patient outcomes together.
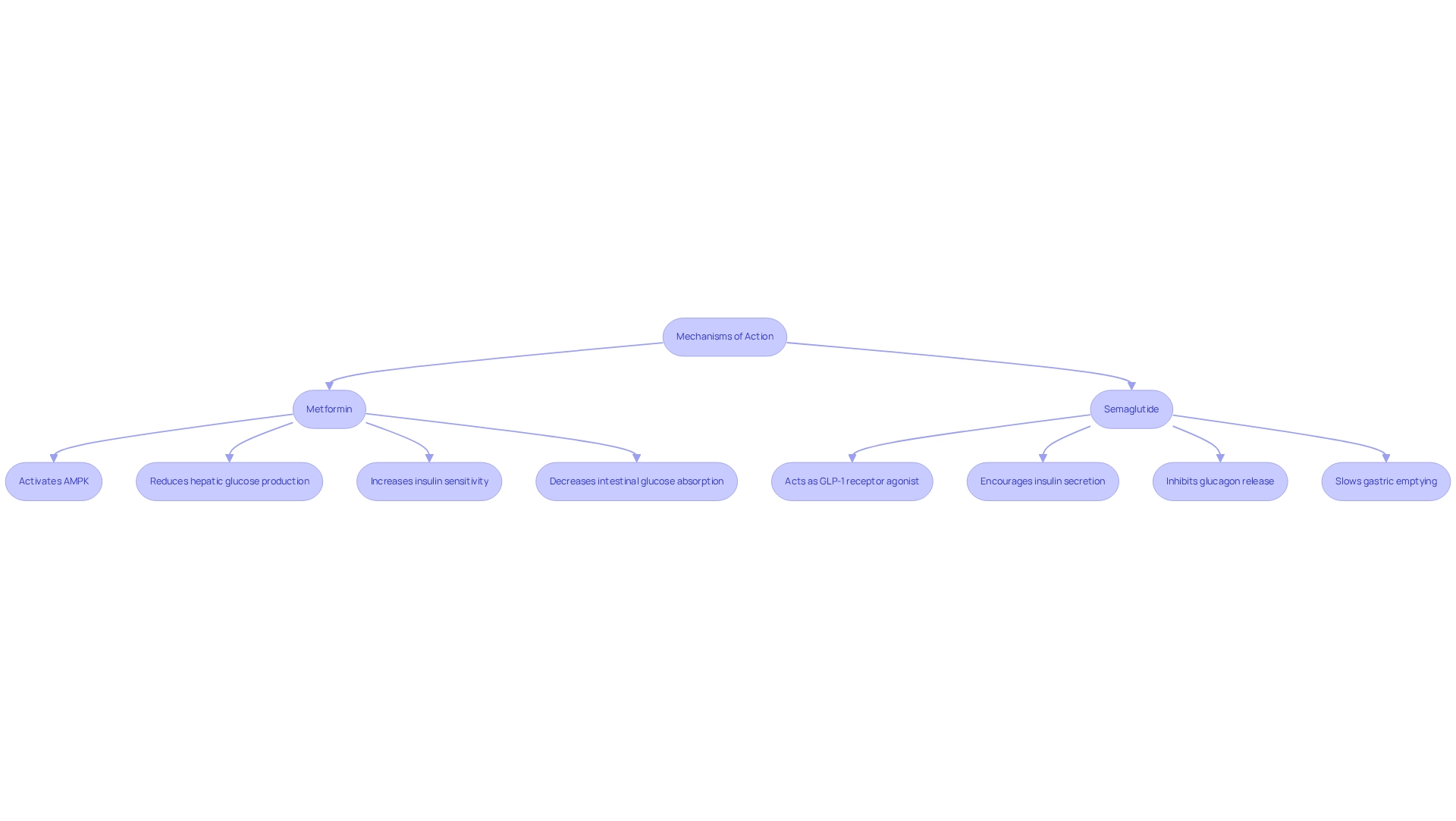
Mechanisms of Action: How Metformin and Semaglutide Work
Managing blood sugar levels can feel overwhelming, but understanding how certain medications work can provide hope and clarity. One such medication activates AMP-activated protein kinase (AMPK), a vital regulator that reduces hepatic glucose production and boosts insulin sensitivity in peripheral tissues. This means it not only promotes glucose uptake in muscles but also decreases intestinal glucose absorption, playing a crucial role in maintaining balanced blood sugar levels. Recent studies have shown that the ability of this medication to activate AMPK is linked to improved insulin sensitivity, which is essential for effective body mass management.
On the other hand, Semaglutide acts as a GLP-1 receptor agonist, mimicking the effects of the GLP-1 hormone. It encourages insulin secretion in a glucose-dependent manner, inhibits glucagon release, and slows down gastric emptying. This dual action not only aids in blood sugar control but also significantly reduces appetite, supporting efforts to decrease body mass. Excitingly, recent studies indicate that the combination of metformin and semaglutide can enhance overall effectiveness, especially for individuals struggling with obesity and insulin resistance. The benefits of this combination are clear. The medication significantly boosts insulin sensitivity, leading to better glucose regulation and reductions in body mass. Many individuals have experienced synergistic effects when using the medication alongside another drug, optimizing their weight loss potential while maintaining a positive safety profile.
In the STEP 5 trial, which evaluated the safety and tolerability of the medication over 104 weeks, gastrointestinal disorders were the most commonly reported adverse events. However, most were mild to moderate, resulting in a low rate of treatment discontinuation. This evidence underscores the promise of combining a diabetes medication with another treatment for improved health outcomes in managing body mass.
Yet, it’s important to acknowledge the limitations of current studies, such as a low percentage of nonwhite participants and a predominance of female participants, which may affect the generalizability of the findings. Additionally, the disruption of GLP-1R has been linked to increased bone resorption and decreased calcitonin expression, highlighting broader implications of GLP-1 receptor activity beyond just body mass reduction. By addressing these factors, we can better understand the joint effectiveness of the medication and another treatment in achieving lasting body mass management. Remember, we’re here for you on this journey, and together, we can achieve your goals.
Efficacy Comparison: Blood Sugar Control and Weight Management
Navigating weight loss can feel overwhelming, and we understand the challenges you face. Clinical studies show that the combination of metformin and semaglutide typically results in a modest reduction in body mass, around 2-3%, while effectively managing blood sugar levels. This makes it a suitable option for those focused on glycemic control. However, if you’re looking for more significant results, Wegovy has shown remarkable efficacy, with studies indicating an average reduction in mass of up to 15% over a 68-week period, along with impressive improvements in HbA1c levels.
As Dr. Timothy Garvey emphasizes, Wegovy is effective and safe for a diverse range of patients with obesity, regardless of age, BMI, or race/ethnicity. This positions it as an ideal choice for individuals seeking substantial weight loss alongside enhanced blood sugar management. Furthermore, recent trials highlight the medication’s ability to decrease cardiovascular events, reinforcing its role in overall health enhancement.
Dr. Domenica Rubino notes that the elevated treatment and trial completion rates were likely influenced by factors like participant retention and motivation, further underscoring the drug’s effectiveness. Additionally, the average change in triglyceride levels was -3.20% with the placebo, showcasing the metabolic advantages of Wegovy compared to other treatments. If you’re pursuing both weight reduction and improved glycemic regulation, this medication may be a more effective choice than metformin and semaglutide.
At Minimal, we believe in a comprehensive approach to health. We combine Wegovy with personalized fitness and nutrition strategies to support your journey toward fat reduction and overall wellness. Administered via a subcutaneous injection once a week, Wegovy is generally well-tolerated, though some common side effects may include nausea, vomiting, upset stomach, and fatigue.
By pairing Semaglutide with a reduced-calorie diet and increased physical activity, we strive to maximize the effectiveness of our programs. Remember, you’re not alone in this journey; together, we can achieve your goals and enhance your health.
Safety Profiles: Side Effects and Contraindications
Metformin is often celebrated for its tolerability, with common side effects primarily involving gastrointestinal disturbances such as nausea and diarrhea. It can aid in fat reduction by diminishing appetite, lessening cravings for high-calorie foods, and reducing the body’s tendency to accumulate fat. While serious adverse effects are infrequent, they can include lactic acidosis, especially in individuals with compromised renal function. It’s important to note that while this medication is effective for weight reduction, it may lead to more severe gastrointestinal issues, including nausea, vomiting, and diarrhea, particularly during the initial dosing phase.
Moreover, there are warnings regarding potential risks of pancreatitis and thyroid tumors, which require careful consideration by healthcare providers. Deliana Infante reminds us, “Semaglutide offers significant benefits; however, it poses potential side effects and risks, with gastrointestinal symptoms being the most frequent side effects.” Recent reports indicate that gastrointestinal symptoms are the most commonly observed side effects for both medications, highlighting the importance of monitoring patient responses.
As we look ahead to 2025, ongoing studies, including the VA-IMPACT trial, are examining the safety profiles of these medications, particularly concerning major adverse cardiovascular events (MACEs) in individuals with pre-diabetes and established atherosclerotic cardiovascular disease (ASCVD). This trial is crucial for understanding the safety profile of these medications in this context. Additionally, the growing popularity of Ozempic, evidenced by Medicare spending of $4.6 million in 2022, underscores its significance in the weight loss medication landscape.
Understanding the safety profiles of metformin and semaglutide is essential for clinicians when prescribing these medications, ensuring that patients receive the most appropriate and effective treatment tailored to their health needs. Insights from case studies, such as Minimal’s holistic health approach, further illustrate the practical application of these medications within a comprehensive care framework. Together, we can navigate these options and find the path that best supports your health journey.
Conclusion
Both Metformin and Semaglutide represent significant advancements in the management of type 2 diabetes, offering unique benefits tailored to different patient needs. Metformin is a foundational treatment, well-regarded for its ability to enhance insulin sensitivity and regulate blood sugar levels, all while maintaining a solid safety profile. Its role in weight management, although modest, complements its primary focus on glycemic control, making it a vital first-line option for many.
On the other hand, Semaglutide stands out with its dual capability of managing blood sugar and promoting substantial weight loss, which is especially beneficial for patients with obesity-related diabetes. Its innovative mechanism as a GLP-1 receptor agonist allows for effective appetite regulation, leading to impressive weight reduction outcomes alongside improved glycemic control. As evidenced by clinical studies, Semaglutide’s efficacy positions it as a compelling choice for individuals seeking significant health improvements.
Understanding the distinct mechanisms, benefits, and potential side effects of these medications is crucial for healthcare providers. This knowledge empowers the development of personalized treatment strategies that optimize patient outcomes while managing safety concerns. As the landscape of diabetes care continues to evolve, integrating these treatments within a comprehensive management plan can truly empower patients to achieve their health goals effectively.
Ultimately, a well-informed approach to diabetes treatment can lead to improved quality of life and better long-term health outcomes for those affected by this condition. Remember, we’re here for you on this journey, and together, we can achieve your goals.
Frequently Asked Questions
What is the key medication for managing type 2 diabetes?
The key medication for managing type 2 diabetes enhances insulin sensitivity and decreases hepatic glucose production. It is recognized for its well-established efficacy and safety profile, making it a preferred first-line treatment among healthcare providers.
What is a GLP-1 receptor agonist and what are its benefits?
A GLP-1 receptor agonist is an injectable medication that aids in blood sugar regulation and promotes significant body mass reduction, which is particularly beneficial for patients with obesity-related diabetes.
What are the benefits of the key medication for diabetes management?
The key medication lowers blood sugar levels, improves insulin sensitivity, reduces the risk of heart disease and diabetic complications, improves long-term A1C levels, and can be taken with or without insulin.
How does the GLP-1 receptor agonist help with weight management?
The GLP-1 receptor agonist regulates blood sugar levels effectively and promotes significant body mass reduction, with many patients reporting reductions of up to 20% when combined with lifestyle changes.
What are the mechanisms of action for the key medication and the GLP-1 receptor agonist?
The key medication primarily enhances the body’s reaction to insulin, while the GLP-1 receptor agonist, along with metformin, imitates incretin hormones that encourage insulin release in response to meals, decreases appetite, and facilitates body mass loss.
What safety concerns are associated with the GLP-1 receptor agonist?
Safety concerns include potential vision problems, gastrointestinal side effects like nausea, vomiting, diarrhea, constipation, abdominal pain, and reduced appetite. It can also cause stomach discomfort, decreased vitamin B12 levels with prolonged use, and in rare instances, lactic acidosis if not used correctly.
How are the two medications utilized in diabetes management?
Both medications play essential roles in diabetes management, each providing distinct advantages that suit various patient profiles. Understanding their differences helps optimize treatment strategies and improve patient outcomes.